Abstract
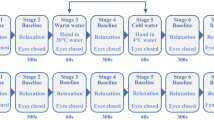
Effects of prolonged photoperiod (18 : 6 model) on the mechanisms regulating microcirculation in the skin were studied in experimental animals. Microcirculation was assessed using laser Doppler flowmetry. It was found that exposure to the prolonged photoperiod regime caused deregulation of blood flow in microvessels, diminishing the amplitudes of endothelial, neurogenic, and myogenic oscillations, and decreased tissue perfusion. The observed hemodynamic abnormalities became more pronounced with longer duration of exposure. Decreased perfusion and progressive impairment of the active factors that regulate microcirculation suggest that exposure to prolonged photoperiod has a negative effect on tissue perfusion, which may be a risk factor for development of cardiovascular diseases.
Similar content being viewed by others
REFERENCES
T. A. leGates, D. C. Fernandez, and S. Hattar, Nat. Rev. Neurosci. 15, 443 (2014). https://doi.org/10.1038/nrn3743
J. Cedernaes, N. Waldeck, and J. Bass, Genes. Dev. 33, 1136 (2019).https://doi.org/10.1101/gad.328633.119
A. Kalsbeek, I. F. Palm, S. E. la Fleur, F. A. J. L. Scheer, S. Perreau-Lenz, M. Ruiter, F. Kreier, C. Cailotto, and R. M. Buijs, J. Biol. Rhythms 21, 458 (2006).https://doi.org/10.1177/0748730406293854
J. F. Duffy and C. A. Czeisler, Sleep. Med. Clin. 4, 165 (2009). https://doi.org/10.1016/j.jsmc.2009.01.004
K. Man, A. Loudon, and A. Chawla, Science (Washington, DC, U. S.) 354, 999 (2016).https://doi.org/10.1126/science.aah4966
C. Scheiermann, J. Gibbs, L. Ince, and A. Loudon, Nat. Rev. Immunol. 18, 423 (2018).https://doi.org/10.1038/s41577-018-0008-4
J. O. Early and A. M. Curtis, Seminars in Immunol. Immunometab. 28, 478 (2016).https://doi.org/10.1016/j.smim.2016.10.006
V. N. Anisimov, I. A. Vinogradova, A. V. Bukalev, et al., Vopr. Onkol. 60 (2), 15 (2014).
V. A. Snezhinskii and N. F. Pobivantseva, Zh. Grodn. Med. Univ., No. 1, 9 (2013).
C. E. Koch, B. Leinweber, B. C. Drengberg, et al., Neurobiol. Stress. 6, 57 (2017).https://doi.org/10.1016/j.ynstr.2016.09.001
K. I. Zhurkin, O. V. Zlobina, A. N. Ivanov, et al., Tromboz, Gemostaz Reol. 3 (67), 164 (2016).
P. Poredos and M. K. Jezovnik, Angiology 7, 564 (2017).
A. N. Ivanov, O. V. Zlobina, K. I. Zhurkin, et al., Region. Krovoobr. Mikrotsirk. 16 (1), 43 (2017).https://doi.org/10.24884/1682-6655-2017-16-1-43-48
O. V. Zlobina, S. S. Pakhomii, I. O. Bugaeva, G. N. Mas-lyakova, and A. N. Ivanov, Vestn. Nov. Med. Tekhnol., Elektron. Izd., No. 5, 245 (2018).
N. E. Tereshkina, O. V. Zlobina, A. N. Ivanov, and A. A. Dolgov, Region. Krovoobr. Mikrotsirk. 3 (67), 129 (2018). https://doi.org/10.24884/1682-6655-2018-17-3-129-134
A. Humeau, A. Koitka, P. Abraham, et al., Phys. Med. Biol. 49, 843 (2004).
A. I. Krupatkin, Region. Krovoobr. Mikrotsirk. 13 (1), 83 (2014).
D. D. Gutterman, D. S. Chabowski, A. O. Kadlec, et al., Circ. Res. 118, 157 (2016). https://doi.org/10.1161/CIRCRESAHA.115.305364
Funding
This work was performed as part of the project “Development of a mathematical model to assess the rate at which functional changes in the body due to light-induced desynchronosis transform into irreversible morphological changes in the target organs in a simulation experiment” according to the State Assignment to the Razumovsky Saratov State Medical University of the Ministry of Health of the Russian Federation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they do not have conflicts of interest.
Additional information
Translated by D. Timchenko
Rights and permissions
About this article
Cite this article
Zlobina, O.V., Pakhomii, S.S., Smolina, E.V. et al. Effect of Photoperiod Duration on Microcirculation in the Skin as Assessed Experimentally by Laser Doppler Flowmetry. Opt. Spectrosc. 129, 857–860 (2021). https://doi.org/10.1134/S0030400X21060205
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0030400X21060205