Abstract
Background
Conventional laparoscopic cholecystectomy (CLC) is regarded as the gold standard for cholecystectomy. However, single-incision laparoscopic cholecystectomy (SLC) has been suggested to replace CLC. This study aimed at comparing long-term incidences of port-site hernia and chronic pain after SLC versus CLC.
Methods
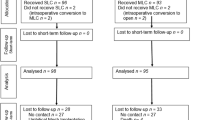
We conducted a matched cohort study based on prospective data (Jan 1, 2009–June 1, 2011) from the Danish Cholecystectomy Database with perioperative information and clinical follow-up. Consecutive patients undergoing elective SLC during the study period were included and matched 1:2 with patients subjected to CLC using pre-defined criteria. Follow-up data were obtained from the Danish National Patient Registry, mailed patient questionnaires, and clinical examination. A port-site hernia was defined as a repair for a port-site hernia or clinical hernia located at one or more port sites.
Results
In total, 699 patients were eligible and 147 patients were excluded from the analysis due to pre-defined criteria. The rate of returned questionnaires was 83%. Thus, 552 (SLC, n = 185; CLC, n = 367) patients were analyzed. The median observation time was 48 months (range 1–65) after SLC and 48 months (1–64) after CLC (P = 0.940). The total cumulated port-site hernia rate was 4 % and 6 % for SLC and CLC, respectively (P = 0.560). Incidences of moderate/severe chronic pain were 4 % and 5 % after SLC and CLC, respectively (P = 0.661).
Conclusions
We found no difference in long-term incidence of port-site hernia or chronic pain after SLC versus CLC.


Similar content being viewed by others
References
Bisgaard T, Kehlet H, Rosenberg J (2001) Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg Acta Chir 167:84–96
Bisgaard T, Klarskov B, Rosenberg J, Kehlet H (2001) Factors determining convalescence after uncomplicated laparoscopic cholecystectomy. Arch Surg 136:917–921
Bisgaard T, Klarskov B, Rosenberg J, Kehlet H (2001) Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain 90:261–269
Keus F, de Jong J a. F, Gooszen HG, van Laarhoven CJHM (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 4:CD006231
Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P (2012) Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc 26:1205–1213
Garg P, Thakur JD, Garg M, Menon GR (2012) Single-incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg 16:1618–1628
Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, Noya G, Boselli C (2013) Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg 100:191–208
Zehetner J, Pelipad D, Darehzereshki A, Mason RJ, Lipham JC, Katkhouda N (2013) Single-access laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Laparosc Endosc Percutan Tech 23:235–243
Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M (2013) Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc 27:2293–2304
Milas M, Deveđija S, Trkulja V (2014) Single incision versus standard multiport laparoscopic cholecystectomy: up-dated systematic review and meta-analysis of randomized trials. Surgeon 12:271–289
Qiu J, Yuan H, Chen S, He Z, Han P, Wu H (2013) Single-port versus conventional multiport laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials and nonrandomized studies. J Laparoendosc Adv Surg Tech A 23:815–831
Harboe KM, Anthonsen K, Bardram L (2009) Validation of data and indicators in the Danish Cholecystectomy Database. Int J Qual Health Care 21:160–168
Møller C, Kehlet H, Utzon J, Ottesen B (2002) Hysterectomy in Denmark. An analysis of postoperative hospitalisation, morbidity and readmission. Dan Med Bull 49:353–357
Schulze S, Iversen MG, Bendixen A, Larsen TS, Kehlet H (2008) Laparoscopic colonic surgery in Denmark 2004–2007. Colorectal Dis 10:869–872
Funch-Jensen P, Bendixen A, Iversen MG, Kehlet H (2008) Complications and frequency of redo antireflux surgery in Denmark: a nationwide study, 1997–2005. Surg Endosc 22:627–630
Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2012) Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg 256:955–958
Owens M, Barry M, Janjua AZ, Winter DC (2011) A systematic review of laparoscopic port site hernias in gastrointestinal surgery. Surgeon 9:218–224
Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T (2011) Low risk of trocar site hernia repair 12 years after primary laparoscopic surgery. Surg Endosc 25:3678–3682
Helgstrand F, Rosenberg J, Bisgaard T (2011) Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia 15:113–121
Comajuncosas J, Hermoso J, Gris P, Jimeno J, Orbeal R, Vallverdú H, López Negre JL, Urgellés J, Estalella L, Parés D (2014) Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: a prospective 3-year follow-up study. Am J Surg 207:1–6
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254:22–27
Jørgensen LN, Rosenberg J, Al-Tayar H, Assaadzadeh S, Helgstrand F, Bisgaard T (2014) Randomized clinical trial of single—versus multi-incision laparoscopic cholecystectomy. Br J Surg 101:347–355
Tranchart H, Ketoff S, Lainas P, Pourcher G, Di Giuro G, Tzanis D, Ferretti S, Dautruche A, Devaquet N, Dagher I (2013) Single incision laparoscopic cholecystectomy: for what benefit? HPB 15:433–438
Krajinovic K, Ickrath P, Germer CT, Reibetanz J (2011) Trocar-site hernia after single-port cholecystectomy: not an exceptional complication? J Laparoendosc Adv Surg Tech A 21:919–921
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237:129–135
Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2014) Long-term recurrence and chronic pain after repair for small umbilical or epigastric hernias: a regional cohort study. Am J Surg. doi:10.1016/j.amjsurg.2014.05.021
Agaba EA, Rainville H, Ikedilo O, Vemulapali P (2014) Incidence of port-site incisional hernia after single-incision laparoscopic surgery. JSLS 18:204–210
Lirici MM, Califano AD, Angelini P, Corcione F (2011) Laparo-endoscopic single site cholecystectomy versus standard laparoscopic cholecystectomy: results of a pilot randomized trial. Am J Surg 202:45–52
Bisgaard T, Klarskov B, Trap R, Kehlet H, Rosenberg J (2002) Microlaparoscopic vs. conventional laparoscopic cholecystectomy: a prospective randomized double-blind trial. Surg Endosc 16:458–464
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24:1842–1848
Asakuma M, Hayashi M, Komeda K, Shimizu T, Hirokawa F, Miyamoto Y, Okuda J, Tanigawa N (2011) Impact of single-port cholecystectomy on postoperative pain. Br J Surg 98:991–995
Chuang SC, Lee KT, Chang WT, Wang SN, Kuo KK, Chen JS, Scheen PC (2004) Risk factors for wound infection after cholecystectomy. J Formos Med Assoc 103:607–612
Murray BW, Cipher DJ, Pham T, Anthony T (2011) The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg 202:558–560
Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, Kono H, Yamamoto H, Ando M, Nagino M (2014) Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg 101:1439–1447
Acknowledgments
Thanks to research nurse Pernille Strandfelt (Bachelor Nurse at the Gastro Unit, Surgical Section, Hvidovre Hospital, University of Copenhagen) for exquisite professional help to carry out the study. No compensation was received for data collection. The study was funded by the University of Copenhagen, the Danish Cholecystectomy Database, and the Danish Hernia database.
Disclosures
Dr. Christoffersen has no conflicts of interest or financial ties to disclose. Dr. Brandt has no conflicts of interest or financial ties to disclose. Dr. Oehlenschläger has no conflicts of interest or financial ties to disclose. Dr. Rosenberg reports grants from Baxter Healthcare, grants from Johnson & Johnson, grants from Bard, personal fees from Bard, and personal fees from Merck, outside the submitted work. Dr. Helgstrand has no conflicts of interest or financial ties to disclose. Dr. Jørgensen declares consultant ships and honoraria from the companies Covidien, Davol and Ethicon, and has no stock ownership, gifts, free or reimbursed travel/vacations, equity interests, arrangements regarding patents or other vested interests. Dr. Bardram has no conflicts of interest or financial ties to disclose. Dr. Bisgaard reports personal fees from Bard, grants from Ethicon, grants from Covidien, and personal fees from Life Cell, outside the submitted work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christoffersen, M.W., Brandt, E., Oehlenschläger, J. et al. No difference in incidence of port-site hernia and chronic pain after single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: a nationwide prospective, matched cohort study. Surg Endosc 29, 3239–3245 (2015). https://doi.org/10.1007/s00464-015-4066-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4066-4