Abstract
Purpose
Specific oral health conditions may be risk factors for breast cancer. This study aimed to investigate the associations of oral health conditions with breast cancer risk.
Methods
A total of 234,363 women from the UK Biobank prospective cohort were included in this study. We examined the association of self-reported painful/bleeding gums, loose teeth, mouth ulcers, toothache, and use of dentures with the risk of breast cancer. Hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the associations were calculated with adjustment for multiple confounders.
Results
No associations of self-reported painful/bleeding gums (HR = 1.04, 95% CI 0.98–1.10), loose teeth (HR = 0.92, 95% CI 0.82–1.02), mouth ulcers (HR = 0.99, 95% CI 0.93–1.06), toothache (HR = 1.03, 95% CI 0.92–1.14), or denture use (HR = 0.96, 95% CI 0.91–1.02) with breast cancer risk were found. No statistical heterogeneity was observed in analyses stratified by baseline smoking and menopausal status.
Conclusion
We observed no association between self-reported oral health conditions with the risk of breast cancer. Additional research with clinical examinations or oral health biomarkers in diverse populations is warranted.
Similar content being viewed by others
Data availability
This research was conducted using the UK Biobank Resource (https://www.ukbiobank.ac.uk/) under Application Number 52576. Data are available from UK Biobank (https://www.ukbiobank.ac.uk/) upon request.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA, Genco RJ (2018) Periodontitis in US adults: National health and nutrition examination survey 2009–2014. J Am Dent Assoc 149:576–88 e6
Dye BA, Weatherspoon DJ, Lopez MG (2019) Tooth loss among older adults according to poverty status in the United States from 1999 through 2004 and 2009 through 2014. J Am Dent Assoc 150:9-23.e3
Shi T, Min M, Sun C, Zhang Y, Liang M, Sun Y (2018) Periodontal disease and susceptibility to breast cancer: a meta-analysis of observational studies. J Clin Periodontol 45:1025–1033
Shao J, Wu L, Leng WD et al (2018) Periodontal disease and breast cancer: a meta-analysis of 1,73,162 participants. Front Oncol 8:601
Jiang X, Shapiro DJ (2014) The immune system and inflammation in breast cancer. Mol Cell Endocrinol 382:673–682
Wu Z, Byrd DA, Wan Y et al (2022) The oral microbiome and breast cancer and nonmalignant breast disease, and its relationship with the fecal microbiome in the Ghana Breast Health Study. Int J Cancer 15:1248
Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr (1998) Microbial complexes in subgingival plaque. J Clin Periodontol 25:134–144
Teles R, Teles F, Frias-Lopez J, Paster B, Haffajee A (2013) Lessons learned and unlearned in periodontal microbiology. Periodontol 62:95–162
Lin D, Yang L, Wen L, Lu H, Chen Q, Wang Z (2021) Crosstalk between the oral microbiota, mucosal immunity, and the epithelial barrier regulates oral mucosal disease pathogenesis. Mucosal Immunol 14:1247–1258
Redfern J, Tosheva L, Malic S, Butcher M, Ramage G, Verran J (2022) The denture microbiome in health and disease: an exploration of a unique community. Lett Appl Microbiol 75:195–209
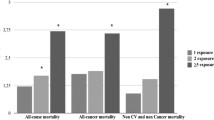
Wu Z, O’Brien KM, Lawrence KG et al (2021) Associations of periodontal disease and tooth loss with all-cause and cause-specific mortality in the Sister Study. J Clin Periodontol 48:1597–1604
Jia M, Wu Z, Vogtmann E et al (2020) The association between periodontal disease and breast cancer in a prospective cohort study. Cancer Prev Res (Phila) 13:1007–1016
Farhat Z, Cadeau C, Eliassen AH, Freudenheim JL (2021) Periodontal disease and breast cancer risk: results from the nurses’ health study. Cancer Epidemiol Biomarkers Prev 30:1757–1760
Kinane DF, Stathopoulou PG, Papapanou PN (2017) Periodontal diseases. Nat Rev Dis Primers 3:17038
Conroy MC, Lacey B, Besevic J et al (2022) UK Biobank: a globally important resource for cancer research. Br J Cancer 128:519
Freudenheim JL, Genco RJ, LaMonte MJ et al (2016) Periodontal disease and breast cancer: prospective cohort study of postmenopausal women. Cancer Epidemiol Biomarkers Prev 25:43–50
Mai X, LaMonte MJ, Hovey KM et al (2016) Periodontal disease severity and cancer risk in postmenopausal women: the buffalo osteoperio study. Cancer Causes Control 27:217–228
Tomar SL, Asma S (2000) Smoking-attributable periodontitis in the United States: findings from NHANES III. J Periodontol 71:743–751
Heer E, Harper A, Escandor N, Sung H, McCormack V, Fidler-Benaoudia MM (2020) Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Glob Health 8:e1027–e1037
Eke PI, Dye BA, Wei L et al (2015) Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 86:611–622
Abbood HM, Hinz J, Cherukara G, Macfarlane TV (2016) Validity of self-reported periodontal disease: a systematic review and meta-analysis. J Periodontol 87:1474–1483
Funding
This work was supported by the Intramural Research Program in the Division of Cancer Epidemiology and Genetics of the National Cancer Institute (NCI) in the US National Institutes of Health (NIH).
Author information
Authors and Affiliations
Contributions
ZW and FL contributed to conducting the analyses. JS aided in data acquisition. EV contributed to study conception and design and supervised the project. ZW drafted the manuscript. GLG and EV contributed to revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare no conflict of interests.
Ethical approval
The UK Biobank has approval from the North West Multi-Centre Research Ethics Committee (MREC) as a Research Tissue Bank (RTB).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, Z., Li, F., Sang, J. et al. The association between poor oral health and risk of breast cancer in the UK Biobank. Cancer Causes Control 34, 491–494 (2023). https://doi.org/10.1007/s10552-023-01682-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01682-2