Abstract
Background
Data on nosocomial bloodstream infections (NBSI) in neurosurgery is limited. This study aimed to analyze the epidemiology, microbiology, outcome, and risk factors for death in neurosurgical patients with NBSI in a multidrug resistant setting.
Methods
Neurosurgical patients with a confirmed NBSI within the period 2003–2012 were retrospectively analyzed. NBSI was diagnosed when a pathogen was isolated from a blood sample obtained after the first 48 h of hospitalization. Patients’ demographic, clinical, and microbiological data were recorded and analyzed using univariate and multivariate analysis.
Results
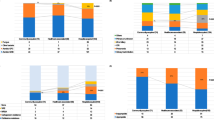
A total of 236 patients with NBSI were identified and 378 isolates were recovered from blood cultures. Incidence of NBSI was 4.3 infections/1000 bed-days. Gram-negative bacteria slightly predominated (54.5 %). The commonest bacteria were coagulase-negative staphylococci (CoNS, 26 %), Klebsiella pneumoniae (15.3 %), Pseudomonas aeruginosa (14.8 %), and Acinetobacter baumannii (13.2 %). Carbapenem resistance was found in 90 % of A. baumannii, in 66 % of P. aeruginosa, and in 22 % (2003–2007) to 77 % (2008–2012) of K. pneumoniae isolates (p < 0.05). Most CoNS and Staphylococcus aureus isolates (94 and 80 %, respectively) were methicillin-resistant. All Gram-negative isolates were sensitive to colistin and all Gram-positive isolates were sensitive to vancomycin and linezolid. Antimicrobial consumption decreased after 2007 (p < 0.05). Overall mortality was 50.4 %. In multivariate analysis, advanced age and stay in an Intermediate Care Unit (IMCU) were independent risk factors for in-hospital mortality (p < 0.05).
Conclusions
Overall, high incidence of NBSI and considerable resistance of Gram-positive and particularly Gram-negative bacteria were noted in neurosurgical patients. Mortality was high with advanced age and stay in IMCU being the most important death-related factors.


Similar content being viewed by others
References
Boque MC, Bodi M, Rello J (2000) Trauma, head injury, and neurosurgery infections. Semin Respir Infect 15:280–286
Dettenkofer M, Ebner W, Hans FJ, Forster D, Babikir R, Zentner J, Pelz K, Daschner FD (1999) Nosocomial infections in a neurosurgery intensive care unit. Acta Neurochir (Wien) 141:1303–1308
Dziedzic T, Slowik A, Szczudlik A (2004) Nosocomial infections and immunity: lesson from brain-injured patients. Crit Care 8:266–270
Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP (1999) Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis 29:239–244
Erdem I, Ozgultekin A, Sengoz Inan A, Ozturk Engin D, Senbayrak Akcay S, Turan G, Dincer E, Oguzoglu N, Goktas P (2009) Bloodstream infections in a medical-surgical intensive care unit: incidence, aetiology, antimicrobial resistance patterns of Gram-positive and Gram-negative bacteria. Clin Microbiol Infect 15:943–946
Falagas ME, Lourida P, Poulikakos P, Rafailidis PI, Tansarli GS (2014) Antibiotic treatment of infections due to carbapenem-resistant Enterobacteriaceae: systematic evaluation of the available evidence. Antimicrob Agents Chemother 58:654–663
Favre B, Hugonnet S, Correa L, Sax H, Rohner P, Pittet D (2005) Nosocomial bacteremia: clinical significance of a single blood culture positive for coagulase-negative staphylococci. Infect Control Hosp Epidemiol 26:697–702
Gocmez C, Celik F, Tekin R, Kamasak K, Turan Y, Palanci Y, Bozkurt F, Bozkurt M (2014) Evaluation of risk factors affecting hospital-acquired infections in the neurosurgery intensive care unit. Int J Neurosci 124:503–508
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Iosifidis E, Antachopoulos C, Tsivitanidou M, Katragkou A, Farmaki E, Tsiakou M, Kyriazi T, Sofianou D, Roilides E (2008) Differential correlation between rates of antimicrobial drug consumption and prevalence of antimicrobial resistance in a tertiary care hospital in Greece. Infect Control Hosp Epidemiol 29:615–622
Kim JM, Park ES, Jeong JS, Kim KM, Oh HS, Yoon SW, Chang HS, Chang KH, Lee SI, Lee MS, Song JH, Kang MW, Park SC, Choe KW, Pai CH (2000) Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Nosocomial Infection Surveillance Committee of the Korean Society for Nosocomial Infection Control. Am J Infect Control 28:454–458
Kourbeti IS, Papadakis JA, Neophytou C, Filippou M, Ioannou A, Karabetsos DA, Bertsias G, Anastasaki M, Vakis AF (2011) Infections in patients with traumatic brain injury who undergo neurosurgery. Br J Neurosurg 25:9–15
Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ (2002) Population-based assessment of intensive care unit-acquired bloodstream infections in adults: incidence, risk factors, and associated mortality rate. Crit Care Med 30:2462–2467
Marchaim D, Zaidenstein R, Lazarovitch T, Karpuch Y, Ziv T, Weinberger M (2008) Epidemiology of bacteremia episodes in a single center: increase in Gram-negative isolates, antibiotics resistance, and patient age. Eur J Clin Microbiol Infect Dis 27:1045–1051
Marra AR, Camargo LF, Pignatari AC, Sukiennik T, Behar PR, Medeiros EA, Ribeiro J, Girao E, Correa L, Guerra C, Brites C, Pereira CA, Carneiro I, Reis M, de Souza MA, Tranchesi R, Barata CU, Edmond MB (2011) Nosocomial bloodstream infections in Brazilian hospitals: analysis of 2,563 cases from a prospective nationwide surveillance study. J Clin Microbiol 49:1866–1871
McLaughlin M, Advincula MR, Malczynski M, Qi C, Bolon M, Scheetz MH (2013) Correlations of antibiotic use and carbapenem resistance in Enterobacteriaceae. Antimicrob Agents Chemother 57:5131–5133
Meyer E, Buttler J, Schneider C, Strehl E, Schroeren-Boersch B, Gastmeier P, Ruden H, Zentner J, Daschner FD, Schwab F (2007) Modified guidelines impact on antibiotic use and costs: duration of treatment for pneumonia in a neurosurgical ICU is reduced. J Antimicrob Chemother 59:1148–1154
Michalopoulos A, Falagas ME, Karatza DC, Alexandropoulou P, Papadakis E, Gregorakos L, Chalevelakis G, Pappas G (2011) Epidemiologic, clinical characteristics, and risk factors for adverse outcome in multiresistant Gram-negative primary bacteremia of critically ill patients. Am J Infect Control 39:396–400
Mitt P, Adamson V, Loivukene K, Lang K, Telling K, Paro K, Room A, Naaber P, Maimets M (2009) Epidemiology of nosocomial bloodstream infections in Estonia. J Hosp Infect 71:365–370
Mouloudi E, Protonotariou E, Zagorianou A, Iosifidis E, Karapanagiotou A, Giasnetsova T, Tsioka A, Roilides E, Sofianou D, Gritsi-Gerogianni N (2010) Bloodstream infections caused by metallo-beta-lactamase/Klebsiella pneumoniae carbapenemase-producing K. pneumoniae among intensive care unit patients in Greece: risk factors for infection and impact of type of resistance on outcomes. Infect Control Hosp Epidemiol 31:1250–1256
No authors. Hellenic Center for Disease Control and Prevention, Ministry of Health (HCDCP). National School of Public Health (NSPH). Accessed April 25 2016
Orsi GB, Scorzolini L, Franchi C, Mondillo V, Rosa G, Venditti M (2006) Hospital-acquired infection surveillance in a neurosurgical intensive care unit. J Hosp Infect 64:23–29
Pournaras S, Protonotariou E, Voulgari E, Kristo I, Dimitroulia E, Vitti D, Tsalidou M, Maniatis AN, Tsakris A, Sofianou D (2009) Clonal spread of KPC-2 carbapenemase-producing Klebsiella pneumoniae strains in Greece. J Antimicrob Chemother 64:348–352
Rupp ME, Archer GL (1994) Coagulase-negative staphylococci: pathogens associated with medical progress. Clin Infect Dis 19:231–243, quiz 244-235
Sablotzki A, Ebel H, Muhling J, Dehne MG, Nopens H, Giesselmann H, Hempelmann G (2000) Dysregulation of immune response following neurosurgical operations. Acta Anaesthesiol Scand 44:82–87
Sostarich AM, Zolldann D, Haefner H, Luetticken R, Schulze-Roebecke R, Lemmen SW (2008) Impact of multiresistance of Gram-negative bacteria in bloodstream infection on mortality rates and length of stay. Infection 36:31–35
Tokars JI (2004) Predictive value of blood cultures positive for coagulase-negative staphylococci: implications for patient care and health care quality assurance. Clin Infect Dis 39:333–341
Tsitsopoulos PP, Iosifidis E, Antachopoulos C, Tsivitanidou M, Anagnostopoulos I, Roilides E, Tsitsopoulos PD (2010) A 5-year epidemiological study of nosocomial bloodstream infections in a neurosurgery department. Infect Control Hosp Epidemiol 31:414–417
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317
Zolldann D, Thiex R, Hafner H, Waitschies B, Lutticken R, Lemmen SW (2005) Periodic surveillance of nosocomial infections in a neurosurgery intensive care unit. Infection 33:115–121
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgments
The authors are thankful to registered nurse Eleni Pappa for contributing to data collection for the years 2007 and 2008.
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Comments
Tsitsopoulos and coworkers have retrospectively analyzed nosocomial bloodstream infections in neurosurgical patients over 10 years in a single-center study with high antimicrobial drug-resistance prevalence. We all have to deal with the problem of an increasing number of one or multiple drug-resistant bacterial infections. I agree with the authors that appropriate studies about this topic seem to be underrepresented for neurosurgical patients. Thus, this 10-year single-center analysis deserves being published in my opinion. The weaknesses of the present study (especially its retrospective design) are adequately discussed by the authors.
Marcus Reinges
Giessen, Germany
Rights and permissions
About this article
Cite this article
Tsitsopoulos, P.P., Iosifidis, E., Antachopoulos, C. et al. Nosocomial bloodstream infections in neurosurgery: a 10-year analysis in a center with high antimicrobial drug-resistance prevalence. Acta Neurochir 158, 1647–1654 (2016). https://doi.org/10.1007/s00701-016-2890-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2890-5