Abstract
Aim
Tuberculosis is a common disease in India with significant morbidity and mortality. Limited data is available on the description of tubercular lymphadenopathy on endoscopic ultrasound.
Methods
Retrospective data of 116 lymph nodes in 113 patients was evaluated at a tertiary care center. Lymphadenopathy in the mediastinum and abdomen were included. The study was aimed at identifying the endoscopic ultrasound (EUS) features of tubercular lymphadenopathy and comparing them with reactive lymphadenopathy in patients with pyrexia of unknown origin.
Results
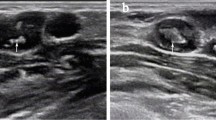
The following features were suggestive of tubercular lymphadenopathy (n = 55) as compared to reactive lymphadenopathy (n = 61): hypoechoic echotexture (94.5 % vs. 75.4 %, p 0.004), patchy anechoic/hypoechoic areas (30.2 % vs. 0 %, p = 0.000), calcification (24.5 % vs. 0 %, p = 0.000), sharply demarcated borders (34.5 % vs. 9.8 %, p = 0.001), pus like material on aspirate (18.2 % vs. 0 %, p 0.000), and conglomeration of lymph nodes (10.9 % vs. 0 %, p = 0.009). The tubercular lymph nodes were significantly larger than reactive nodes at long axis and short axis diameter (2.4 ± 1.1 vs. 1.6 ± 0.6 cm, p < 0.001 and 1.5 ± 0.7 vs. 0.9 ± 0.3 cm, p = 0.001 respectively). On cytopathological examination, presence of necrosis (92.7 % vs. 0 %, p = 0.000) and granulomas (78.1 % vs. 0 %, p = 0.000) favored tubercular as compared to reactive lymphadenopathy.
Conclusion
EUS features like hypoechoic echotexture, patchy anechoic/hypoechoic areas, calcification, sharply demarcated borders, conglomeration, purulent aspirate, larger size, and cytopathological presence of necrosis/granulomas are suggestive of tubercular as compared to reactive lymphadenopathy.




Similar content being viewed by others
References
Kent DC. Tuberculous lymphadenitis: not a localized disease process. Am J Med Sci. 1967;254:866–74.
Shivpuri DN, Ban B. Tuberculoushilar and mediastinal adenitis: course, prognosis, and ambulatory chemotherapy. Am Rev Tuberc. 1957;76:799–810.
Bandyopadhyay D, Bandyopadhyay R, Paul R, Roy D. Etiological study of fever of unknown origin in patients admitted to medicine ward of a teaching hospital of eastern India. J Glob Infect Dis. 2011;3:329–33.
Gupta S, Rajak CL, Sood BP, Gulati M, Rajwanshi A, Suri S. Sonographically guided fine needle aspiration biopsy of abdominal lymph nodes: experience in 102 patients. J Ultrasound Med. 1999;18:135–9.
Avritscher R, Krishnamurthy S, Ensor J, et al. Accuracy and sensitivity of computed tomography-guided percutaneous needle biopsy of pulmonary hilar lymphnodes. Cancer. 2010;116:1974–80.
Rana SS, Bhasin DK, Srinivasan R, Singh K. Endoscopic ultrasound (EUS) features of mediastinal tubercular lymphadenopathy. Hepatogastroenterology. 2011;58:819–23.
Puri R, Mangla R, Eloubeidi M, Vilmann P, Thandassery R, Sud R. Diagnostic yield of EUS-guided FNA and cytology in suspected tubercular intra-abdominal lymphadenopathy. Gastrointest Endosc. 2012;75:1005–10.
Puri R, Vilmann P, Sud R, et al. Endoscopic ultrasound-guided fine-needle aspiration cytology in the evaluation of suspected tuberculosis in patients with isolated mediastinal lymphadenopathy. Endoscopy. 2010;42:462–7.
Dhir V, Mathew P, Bhandari S, et al. Endosonography-guided fine needle aspiration cytology of intra-abdominal lymph nodes with unknown primary in a tuberculosis endemic region. J Gastroenterol Hepatol. 2011;26:1721–4.
Rana SS, Bhasin DK, Rao C, Srinivasan R, Singh K. Tuberculosis presenting as dysphagia: clinical, endoscopic, radiological and endosonographic features. Endosc Ultrasound. 2013;2:92–5.
Song HJ, Park YS, Seo DW, et al. Diagnosis of mediastinal tuberculosis by using EUS-guided needle sampling in a geographic region with an intermediate tuberculosis burden. Gastrointest Endosc. 2010;71:1307–13.
Song TJ, Lee SS, Park do H, et al. Yield of EUS-guided FNA on the diagnosis of pancreatic/peripancreatic tuberculosis. Gastrointest Endosc. 2009;69:484–91.
Singh KK, Tyagi JS, Muralidhar M, et al. Comparison of in house polymerase chain reaction with conventional techniques for the detection of Mycobacterium tuberculosis DNA in granulomatous lymphadenopathy. J Clin Pathol. 2000;53:355–61.
Portillo-Gómez L, Murillo-Neri MV, Gaitan-Mesa J, Sosa-Iglesias EG. Nested polymerase chain reaction in the diagnosis of cervical tuberculous lymphadenitis in Mexican children. Int J Tuberc Lung Dis. 2008;12:1313–9.
Pahwa R, Hedau S, Jain S, et al. Assessment of possible tuberculous lymphadenopathy by PCR compared to non-molecular methods. J Med Microbiol. 2005;54:873–8.
Patwardhan SA, Bhargava P, Bhide VM, Kelkar DS. A study of tubercular lymphadenitis: a comparison of various laboratory diagnostic modalities with a special reference to tubercular polymerase chain reaction. Indian J Med Microbiol. 2011;29:389–94.
Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015;78:47–55.
Lee JS, Kim EC, Joo SI, et al. The incidence and clinical implication of sputum with positive acid-fast bacilli smear but negative in mycobacterial culture in a tertiary referral hospital in South Korea. J Korean Med Sci. 2008;23:767–71.
Acknowledgments
Mr Vipin Thomas, Mr Manish (statistical help), Mr Yogesh Saini
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
VB, NSC, RP, NK, RR, MN, RRS, HS, MG, and RS declare that they have no conflict of interest.
Ethics statement
The authors declare that the study was performed in a manner to conform to the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning Human and Animal Rights, and the authors followed the policy concerning Informed Consent as shown at Springer.com.
Rights and permissions
About this article
Cite this article
Bodh, V., Choudhary, N.S., Puri, R. et al. Endoscopic ultrasound characteristics of tubercular lymphadenopathy in comparison to reactive lymph nodes. Indian J Gastroenterol 35, 55–59 (2016). https://doi.org/10.1007/s12664-016-0627-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-016-0627-2