Abstract
Introduction
Post-transplant relapse is a major factor influencing the long-term outcome in alcoholic liver disease (ALD) patients.
Aims
The aim of this study was to evaluate the relapse rates following living donor liver transplantation (LDLT) in patients with ALD in the Indian context with strong family support.
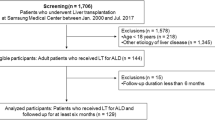
Methods
Of 458 patients who underwent LDLT for ALD, 408 were included in the study. Post-transplant relapse was determined by information provided by the patient and/or family by means of outpatient and e-mail questionnaire, supported by clinical/biochemical parameters/liver histopathology.
Results
All except one were males, with a mean age of 46.9 ± 8.5 years. The overall rate of relapse was 9.5 % at 34.7 months (interquartile range (IQR) 15–57.6), lower than that reported in the literature from the West. The relapse rate was higher in patients with a shorter duration of pre-transplant abstinence (17.4 % and 15.4 % for recipients with pre-transplant abstinence of <3 and <6 months, respectively, p < 0.05). The overall survival was 88.5 % at 3 years. Of 39 patients with relapse, 16 (41 %) were occasional drinkers, 14 (35.8 %) were moderate drinkers, and 9 (23 %) were heavy drinkers. All the heavy drinkers presented with features of graft dysfunction.
Conclusions
Good results can be obtained following LDLT for ALD, with significantly lower relapse rates in our setup as compared to the West.


Similar content being viewed by others
References
Starzl TE, Van Thiel O, Tzakis AG, et al. Orthotopic liver transplantation for alcoholic cirrhosis. JAMA. 1988;260:2542–4.
Neuberger J, James O. Guidelines for selection of patients for liver transplantation in the era of donor-organ shortage. Lancet. 1999;354:1636–9.
Kelly M, Chick J, Gribble R, et al. Predictors of relapse to harmful alcohol after orthotopic liver transplantation. Alcohol. 2006;41:278–83.
Lim JK, Keeffe EB. Liver transplantation for alcoholic liver disease: current concepts and length of sobriety. Liver Transpl. 2004;10 10 Suppl 2:S31–8.
Pageaux GP, Bismuth M, Perney P, et al. Alcohol relapse after liver transplantation for alcoholic liver disease: does it matter? J Hepatol. 2003;38:629–34.
Gish RG, Lee A, Brooks L, et al. Long-term follow-up of patients diagnosed with alcohol dependence or alcohol abuse who were evaluated for liver transplantation. Liver Transpl. 2001;7:581–7.
Poynard T, Naveau S, Doffoel M, et al. Evaluation of efficacy of liver transplantation in alcoholic cirrhosis using matched and simulated controls: 5-year survival. Multi-centre group. J Hepatol. 1999;30:1130–7.
Lucey MR, Schaubel DE, Guidinger MK, et al. Effect of alcoholic liver disease and hepatitis C infection on waiting list and post-transplant mortality and transplant survival benefit. Hepatology. 2009;50:400–6.
Mackie J, Groves K, Hoyle A, et al. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transpl. 2001;7:418–27.
Bird GL, O’Grady JG, Harvey FA, Calne RY, Williams R. Liver transplantation in patients with alcoholic cirrhosis: selection criteria and rates of survival and relapse. BMJ. 1990;301:15–7.
Orsorio RW, Ascher NL, Avery M, Bacchetti P, Roberts JP, Lake JR. Predicting recidivism after liver transplantation for alcoholic liver disease. Hepatology. 1994;20:105–10.
Kumar S, Stauber RE, Gavaler JS, et al. Orthotopic liver transplantation for alcoholic liver disease. Hepatology. 1990;11:159–64.
Bellamy CO, DiMartini AM, Ruppert K, et al. Liver transplantation for alcoholic cirrhosis: long term follow-up and impact of disease recurrence. Transplantation. 2001;72:619–26.
Mathurin P, Moreno C, Samuel D, et al. Early liver transplantation for alcoholic hepatitis. N Engl J Med. 2011;365:1790–800.
McMaster P. Transplantation for alcoholic liver disease in an era of organ shortage. Lancet. 2000;355:424–5.
Louvet A, Naveau S, Abdelnour M, et al. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348–54.
Perney P, Bismuth M, Sigaud H, et al. Are preoperative patterns of alcohol consumption predictive of relapse after liver transplantation for alcoholic liver disease? Transpl Int. 2005;18:1292–7.
Björnsson E, Olsson J, Rydell A, et al. Long-term follow-up of patients with alcoholic liver disease after liver transplantation in Sweden: impact of structured management on recidivism. Scand J Gastroenterol. 2005;40:206–16.
DiMartini A, Day N, Dew MA, et al. Alcohol consumption patterns and predictors of use following liver transplantation for alcoholic liver disease. Liver Transpl. 2006;12:813–20.
Pfitzmann R, Schwenzer J, Rayes N, Seehofer D, Neuhaus R, Nüssler NC. Long-term survival and predictors of relapse after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl. 2007;13:197–205.
De Gottardi A, Spahr L, Gelez P, et al. A simple score for predicting alcohol relapse after liver transplantation: results from 387 patients over 15 years. Arch Intern Med. 2007;167:1183–8.
Gedaly R, McHugh PP, Johnston TD, et al. Predictors of relapse to alcohol and illicit drugs after liver transplantation for alcoholic liver disease. Transplantation. 2008;86:1090–5.
Tandon P, Goodman KJ, Ma MM, et al. A shorter duration of pre-transplant abstinence predicts problem drinking after liver transplantation. Am J Gastroenterol. 2009;104:1700–6.
Karim Z, Intaraprasong P, Scudamore CH, et al. Predictors of relapse to significant alcohol drinking after liver transplantation. Can J Gastroenterol. 2010;24:245–50.
Hartl J, Scherer MN, Loss M, et al. Strong predictors for alcohol recidivism after liver transplantation: nonacceptance of the alcohol problem and abstinence of <3 months. Scand J Gastroenterol. 2011;46:1257–66.
Rodrigue JR, Hanto DW, Curry MP. The alcohol relapse risk assessment: a scoring system to predict the risk of relapse to any alcohol use after liver transplant. Prog Transplant. 2013;23:310–8.
Deruytter E, Van Steenkiste CV, Trepo E. Liver transplantation for alcoholic liver disease: a retrospective analysis of recidivism, survival and risk factors predisposing to alcohol relapse. Acta Gastroenterol Belg. 2013;76:282–90.
Egawa H, Nishimura K, Teramukai S, et al. Risk factors for alcohol relapse after liver transplantation for alcoholic cirrhosis in Japan. Liver Transpl. 2014;20:298–310.
Kawaguchi Y, Sugawara Y, Yamashiki N, et al. Role of 6-month abstinence rule in living donor liver transplantation for patients with alcoholic liver disease. Hepatol Res. 2013;43:1169–74.
Choudhary NS, Tomar M, Chawla YK, et al. Hepatic osteodystrophy is common in patients with noncholestatic liver disease. Dig Dis Sci. 2011;56:3323–7.
Duseja A, Choudhary NS, Gupta S, Dhiman RK, Chawla Y. APACHE II score is superior to SOFA, CTP and MELD in predicting the short-term mortality in patients with acute-on-chronic liver failure (ACLF). J Dig Dis. 2013;14:484–90.
Jauhar S, Talwalkar JA, Schneekloth T, Jowsey S, Wiesner RH, Menon KV. Analysis of factors that predict alcohol relapse following liver transplantation. Liver Transpl. 2004;10:408–11.
Acknowledgments
The authors thank Mr. Yogesh Saini (clinical research coordinator) and Mr. Manish (bio-statistician) for their help in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SS, NSC, SKY, NS, NK, RR, SM, VR, AR, SG, PB, SKR, VR, DG, and ASS declare that they have no conflict of interest.
Ethics statement
The authors declare that the study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Rights and permissions
About this article
Cite this article
Saigal, S., Choudhary, N.S., Yadav, S.K. et al. Lower relapse rates with good post-transplant outcome in alcoholic liver disease: Experience from a living donor liver transplant center. Indian J Gastroenterol 35, 123–128 (2016). https://doi.org/10.1007/s12664-016-0646-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-016-0646-z