Abstract
Purpose
Uncertainty exists regarding Patient-Reported Outcomes (PROs) and Health-Related Quality of Life (HRQoL) of patients with metastatic colorectal cancer (mCRC) treated with cetuximab or bevacizumab. We conducted a prospective cohort study comparing PROs and HRQoL from both therapies.
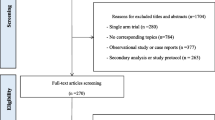
Methods
We assessed PROs and HRQoL from patients treated with cetuximab or bevacizumab using QLQ-C30 and QLQ-CR29 questionnaires at three sequential time points, including baseline. Global Health Status (GHS), functional and symptom scales, and Overall Treatment Utility (derived from clinical and patient-reported outcomes) were compared for the two treatment strategies.
Results
Between January 2017 and April 2018, 44 patients were allocated to cetuximab (n = 19) or bevacizumab (n = 25). Except for RAS mutation status, patient baseline characteristics were generally well balanced across treatment groups. A higher proportion of patients experienced a deterioration in GHS (≥ 10%) in cetuximab arm − 53.8% (95% CI 25.1–80.8%) at 6 weeks and 66.7% (95% CI 29.9–92.5%) at 12 weeks—comparing to bevacizumab cohort: 18.2% (95% CI 5.2–40.3%) at 6 weeks and 12.5% (95% CI:1.6–38.3%) at 12 weeks. Treatment utility rates at 6 and 12 weeks were, respectively, 88.6% and 69.8% for bevacizumab, compared to 49% and 19.1% for cetuximab (p = 0.004), a difference confirmed in subset analyses.
Conclusions
In patients with mCRC, cetuximab-containing regimens led to a progressive negative impact on PROs and global HRQoL, when compared to baseline and bevacizumab. Future research is needed to confirm these results. Our findings demonstrate the value of PROs when assessing comparative effectiveness of different treatment regimens.





Similar content being viewed by others
References
Atkinson TM, Ryan SJ, Bennett AV, Stover AM, Saracino RM, Rogak LJ, Jewell ST, Matsoukas K, Li Y, Basch E (2016) The Association between Clinician-Based Common Terminology Criteria for Adverse Events (CTCAE) and Patient-Reported Outcomes (PRO): a systematic review. Support Care Cancer 24(8):3669–3676. https://doi.org/10.1007/s00520-016-3297-9
Basch E (2010) The missing voice of patients in drug-safety reporting. N Engl J Med 362(10):865–869. https://doi.org/10.1056/NEJMp1002530
Bottomley A, Pe M, Sloan J, Basch E, Bonnetain F, Calvert M, Campbell A et al (2016) Analysing data from patient-reported outcome and quality of life endpoints for cancer clinical trials: a start in setting international standards. Lancet Oncol 17(11):e510–e514. https://doi.org/10.1016/S1470-2045(16)30510-1
Burgess S, S DS, Thompson SG (2017) A Review of instrumental variable estimators for mendelian randomization. Stat Methods Med Res 26(5):2333–2355. https://doi.org/10.1177/0962280215597579
Calvert M, Kyte D, Mercieca-Bebber R, Slade A, Chan AW, King MT (2018) Guidelines for inclusion of patient-reported outcomes in clinical trial protocols the spirit-pro extension. J Am Med Assoc 319(5):483–494. https://doi.org/10.1001/jama.2017.21903
Cherny NI, Sullivan R, Dafni U, Kerst JM, Sobrero A, Zielinski C, de Vries EGE, Piccart MJ (2015) A standardised, generic, validated approach to stratify the magnitude of clinical benefit that can be anticipated from anti-cancer therapies: The European Society for Medical Oncology Magnitude of Clinical Benefit Scale (ESMO-MCBS). Ann Oncol 26(8):1547–1573. https://doi.org/10.1093/annonc/mdv249
Cremolini C, Loupakis F, Antoniotti C, Lupi C, Sensi E, Lonardi S, Mezi S et al (2015) FOLFOXIRI plus Bevacizumab versus FOLFIRI plus Bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analyses of the open-label, phase 3 TRIBE study. Lancet Oncol 16(13):1306–1315. https://doi.org/10.1016/S1470-2045(15)00122-9
Di Maio M, Gallo C, Leighl NB, Piccirillo MC, Daniele G, Nuzzo F, Gridelli C et al (2015) Symptomatic toxicities experienced during anticancer treatment: agreement between patient and physician reporting in three randomized trials. J Clin Oncol 33(8):910–915. https://doi.org/10.1200/JCO.2014.57.9334
Di Maio M, Basch E, Bryce J, Perrone F (2016) Patient-reported outcomes in the evaluation of toxicity of anticancer treatments. Nat Rev Clin Oncol 13(5):319–325. https://doi.org/10.1038/nrclinonc.2015.222
Elez E, Argilés G, Tabernero J (2015) First-line treatment of metastatic colorectal cancer: interpreting FIRE-3, PEAK, and CALGB/SWOG 80405. Curr Treat Options Oncol 16(11):52. https://doi.org/10.1007/s11864-015-0369-x
European Organisation for Research and Treatment of Cancer Quality of Life Department (n.d.) EORTC QLQ-C30 Quality of Life Questionnaire Version 3.0. http://groups.eortc.be/qol/eortc-qlq-c30
European Organisation for Research and Treatment of Cancer Quality of Life Department (n.d.) EORTC Quality of Life Questionnaire Colorectal Module (QLQ-CR29) Version 2.1. http://groups.eortc.be/qol/why-do-we-need-modules
Fallowfield LJ, Fleissig Anne (2012) The value of progression-free survival to patients with advanced-stage cancer. Nat Rev Clin Oncol 9(1):41–47. https://doi.org/10.1038/nrclinonc.2011.156
Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, Allen C, Alsharif U et al (2018) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 Cancer Groups, 1990 to 2016. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2018.2706
Groenvold M, Klee MC, Sprangers MA, Aaronson NK (1997) Validation of the EORTC QLQ-C30 quality of life questionnaire through combined qualitative and quantitative assessment of patient-observer agreement. J Clin Epidemiol 50(4):441–450
Hegewisch-Becker S, Nöpel-Dünnebacke S, Hinke A, Graeven U, Reinacher-Schick A, Hertel J, Lerchenmüller CA et al (2018) Impact of primary tumour location and RAS/BRAF mutational status in metastatic colorectal cancer treated with first-line regimens containing oxaliplatin and bevacizumab: prognostic factors from the AIO KRK0207 first-line and maintenance therapy trial. Eur J Cancer 101:105–113. https://doi.org/10.1016/j.ejca.2018.06.015
Heinemann V, Von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran S-E, Heintges T, Lerchenmüller C, Kahl C (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as Fi Rst-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 15:1065–1075
Kaasa S, Loge JH, Aapro M, Albreht T, Anderson R, Bruera E, Brunelli C et al (2018) Integration of oncology and palliative care: a lancet oncology commission. Lancet Oncol 2045(18):1–66. https://doi.org/10.1016/S1470-2045(18)30415-7
Kluetz PG, O’Connor DJ, Soltys K (2018) Incorporating the patient experience into regulatory decision making in the USA, Europe, and Canada. Lancet Oncol 19(5):e267–e274. https://doi.org/10.1016/S1470-2045(18)30097-4
LeBlanc TW, Abernethy AP (2017) Patient-reported outcomes in cancer care-hearing the patient voice at greater volume. Nat Rev Clin Oncol 14(12):763–772. https://doi.org/10.1038/nrclinonc.2017.153
Marques RP, Duarte GS, Sterrantino C, Pais HL, Quintela A, Martins AP, Costa J (2017) Triplet (FOLFOXIRI) versus doublet (FOLFOX or FOLFIRI) backbone chemotherapy as first-line treatment of metastatic colorectal cancer: a systematic review and meta-analysis. Crit Rev Oncol/Hematol 118(10):54–62. https://doi.org/10.1016/j.critrevonc.2017.08.006
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16(1):139–144. https://doi.org/10.1200/JCO.1998.16.1.139
Porter ME (2010) What is value in health care? N Engl J Med 363(26):2477–2481
Rees JR, Whale K, Fish D, Fayers P, Cafaro V, Pusic A, Blazeby JM, Efficace F (2015) Patient-reported outcomes in randomised controlled trials of colorectal cancer: an analysis determining the availability of robust data to inform clinical decision-making. J Cancer Res Clin Oncol 141(12):2181–2192. https://doi.org/10.1007/s00432-015-1970-x
Schnipper LE, Davidson NE, Wollins DS, Blayney DW, Dicker AP, Ganz PA, Hoverman JR et al (2016) Updating the American Society of Clinical Oncology Value Framework: revisions and reflections in response to comments received. J Clin Oncol 34(24):2925–2933. https://doi.org/10.1200/JCO.2016.68.2518
Schwartzberg LS, Rivera F, Karthaus M, Fasola G, Canon J-L, Hecht JR, Yu H, Oliner KS, Go WY (2014) PEAK: a randomized, multicenter phase ii study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (MFOLFOX6) or bevacizumab plus MFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal. J Clin Oncol 32(21):2240–2247. https://doi.org/10.1200/JCO.2013.53.2473
Secord AA, Coleman RL, Havrilesky LJ, Abernethy AP, Samsa GP, Cella D (2015) Patient-reported outcomes as end points and outcome indicators in solid tumours. Nat Rev Clin Oncol 12(6):358–370. https://doi.org/10.1038/nrclinonc.2015.29
Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A (2017) Colorectal cancer statistics, 2017. CA Cancer J Clin 67(3):177–193. https://doi.org/10.3322/caac.21395
Snyder CF, Herman JM, White SM, Luber BS, Blackford AL, Carducci MA, Albert WW (2014) When using patient-reported outcomes in clinical practice, the measure matters: a randomized controlled trial. J Oncol Pract 10(5):e299–e306. https://doi.org/10.1200/JOP.2014.001413
Snyder CF, Blackford AL, Sussman J, Bainbridge D, Howell D, Seow HY, Carducci MA, Albert WW (2015) Identifying changes in scores on the EORTC-QLQ-C30 representing a change in patients’ supportive care needs. Qual Life Res 24(5):1207–1216. https://doi.org/10.1007/s11136-014-0853-y
Uwer L, Rotonda C, Guillemin F, Miny J, Kaminsky M-C, Mercier M, Tournier-Rangeard L et al (2011) Responsiveness of EORTC QLQ-C30, QLQ-CR33 and FACT-C quality of life questionnaires in patients with colorectal cancer. Health Qual Life Outcomes 9(1):70. https://doi.org/10.1186/1477-7525-9-70
Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, Aranda Aguilar E et al (2016) ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. https://doi.org/10.1093/annonc/mdw235
Velikova G, Coens C, Efficace F, Greimel E, Groenvold M, Johnson C, Singer S, van de Poll-Franse L, Young T, Bottomley A (2012) Health-related quality of life in EORTC clinical trials—30 years of progress from methodological developments to making a real impact on oncology practice. Eur J Cancer Suppl 10(1):141–149. https://doi.org/10.1016/S1359-6349(12)70023-X
Venook AP, Niedzwiecki D, Lenz H-J, Innocenti F, Fruth B, Meyerhardt JA, Schrag D et al (2017) Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients With KRAS wild-type advanced or metastatic colorectal cancer. J Am Med Assoc 317(23):2392. https://doi.org/10.1001/jama.2017.7105
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Whistance RN, Conroy T, Chie W, Costantini A, Sezer O, Koller M, Johnson CD et al (2009) Clinical and psychometric validation of the EORTC QLQ-CR1 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer (Oxford, England : 1990) 45(17):3017–3026. https://doi.org/10.1016/j.ejca.2009.08.014
Wille-Jørgensen P, Syk In, Smedh K, Laurberg S, Nielsen DT, Petersen SH, Renehan AG, Horváth-Puho E, Påhlman L, Sørensen HT (2018) Effect of more vs less frequent follow-up testing on overall and colorectal cancer-specific mortality in patients with stage II or III colorectal cancer the COLOFOL randomized clinical trial. J Am Med Assoc 319(20):2095–2103. https://doi.org/10.1001/jama.2018.5623
Wilson TR, Yvonne B, David JA (2012) Pitfalls in the interpretation of standardised quality of life instruments for individual patients? a qualitative study in colorectal cancer. Qual Life Res. https://doi.org/10.1007/s11136-012-0303-7
Wong CKH, Chen J, Yu CLY, Sham M, Lam CLK (2015) Systematic review recommends the European Organization for Research and Treatment of Cancer colorectal cancer-specific module for measuring quality of life in colorectal cancer patients. J Clin Epidemiol 68(3):266–278. https://doi.org/10.1016/j.jclinepi.2014.09.021
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RPM and APM conceived, designed, and planned the study. RPM led the study assessments and data acquisition process. HLP and AQ provided expertise on metastatic colorectal cancer and contributed to data acquisition. RPM interpreted and discussed the results. PH performed the statistical analysis, interpreted, and discussed the results. RPM and PH contributed to drafting of the manuscript. All authors read, provided feedback, and approved the final manuscript. All authors had full access to all of the data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approved by local committee.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marques, R.P., Heudtlass, P., Pais, H.L. et al. Patient-reported outcomes and health-related quality of life for cetuximab versus bevacizumab in metastatic colorectal cancer: a prospective cohort study. J Cancer Res Clin Oncol 145, 1719–1728 (2019). https://doi.org/10.1007/s00432-019-02924-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-02924-0