Abstract
Purpose
The circulating level of adipocyte fatty acid–binding protein (AFABP), a biomarker with prognostic and therapeutic importance in metabolic disorders, has been shown to be elevated in obstructive sleep apnea (OSA). This randomized controlled study aimed to investigate the effect of continuous positive airway pressure (CPAP) treatment for OSA on AFABP levels.
Methods
Consecutive subjects attending sleep study were invited if they were confirmed to have severe OSA and were free of metabolic diseases. Participants were randomized (1:1) into CPAP or observation group for 4 weeks. Demographics, anthropometric data, and circulating biomarkers were checked at baseline and after the 4-week study period.
Results
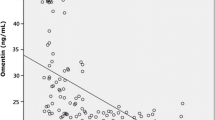
Ninety subjects were randomized. The mean age was 46 ± 9 years old; 82% were male. Their mean body mass index (BMI) was 29 ± 5 kg/m2. By intention-to-treat approach, the CPAP group showed significant reductions in Epworth sleepiness scale and morning systolic blood pressure (− 7.2 mmHg, − 12.7 to − 1.7 mmHg, p = 0.011), but no significant difference in AFABP, adiponectin, C-reactive protein (CRP), and 8-isoprostane levels. In the per-protocol analysis, when only those who were compliant to CPAP were included, a significant reduction in AFABP (− 7.32 ng/ml, − 13.58, − 1.06, p = 0.023) were found in the CPAP-treated group compared with the control group, along with improvements in clinical parameters. Changes in AFABP were independently associated with both systolic blood pressure (β = 0.289, p = 0.028) and diastolic blood pressure (β = 0.217, p = 0.030).
Conclusion
CPAP therapy used regularly over 4 weeks for severe OSA lowered circulating AFABP level, suggesting a potential beneficial effect of OSA treatment on alleviating metabolic risks.
Trial registration
The research protocol was registered at the National Institutes of Health clinical trials registry (NCT01173432).

Similar content being viewed by others
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014
Lam DC, Lam KS, Ip MS (2015) Obstructive sleep apnoea, insulin resistance and adipocytokines. Clin Endocrinol 82(2):165–177
Canto Gde L, Pacheco-Pereira C, Aydinoz S, Major PW, Flores-Mir C, Gozal D (2015) Biomarkers associated with obstructive sleep apnea: a scoping review. Sleep Med Rev 23:28–45
Kralisch S, Fasshauer M (2013) Adipocyte fatty acid binding protein: a novel adipokine involved in the pathogenesis of metabolic and vascular disease? Diabetologia. 56(1):10–21
Xu A, Vanhoutte PM (2012) Adiponectin and adipocyte fatty acid binding protein in the pathogenesis of cardiovascular disease. Am J Physiol Heart Circ Physiol 302(6):H1231–H1240
Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH et al (2007) Circulating adipocyte-fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulation. 115(12):1537–1543
Lee CH, Cheung CYY, Woo YC, Lui DTW, Yuen MMA, Fong CHY, Chow WS, Xu A, Lam KSL (2018) Circulating adipocyte fatty acid-binding protein concentrations predict multiple mortality outcomes among men and women with diabetes. Clin Chem 64(10):1496–1504
Lam DC, Xu A, Lam KS, Lam B, Lam JC, Lui MM et al (2009) Serum adipocyte-fatty acid binding protein level is elevated in severe OSA and correlates with insulin resistance. Eur Respir J 33(2):346–351
Bhushan B, Khalyfa A, Spruyt K, Kheirandish-Gozal L, Capdevila OS, Bhattacharjee R et al (2011) Fatty-acid binding protein 4 gene polymorphisms and plasma levels in children with obstructive sleep apnea. Sleep Med 12(7):666–671
Balci MM, Arslan U, Firat H, Kocaoglu I, Vural MG, Balci KG et al (2012) Serum levels of adipocyte fatty acid-binding protein are independently associated with left ventricular mass and myocardial performance index in obstructive sleep apnea syndrome. J Investig Med 60(7):1020–1026
Wang YB, Li XF, Chen R, Shen JH, Zhang YH (2017) Association between serum adipocyte fatty acid binding protein level and insulin resistance in patients with OSAS. Zhonghua Yi Xue Za Zhi 97(48):3779–3782
Catala R, Cabre A, Hernandez-Flix S, Ferre R, Sangenis S, Plana N et al (2013) Circulating FABP4 and FABP5 levels are differently linked to OSA severity and treatment. Sleep 36(12):1831–1837
Sovova E, Hobzova M, Stejskal D, Sova M, Kolek V, Zapletalova J (2012) Treatment of obstructive sleep apnea with continuous positive airway pressure decreases adipocyte fatty acid-binding protein levels. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 156(1):58–62
Lui MM, Lam JC, Mak HK, Xu A, Ooi C, Lam DC et al (2009) C-reactive protein is associated with obstructive sleep apnea independent of visceral obesity. Chest. 135(4):950–956
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178
Furuhashi M, Saitoh S, Shimamoto K, Miura T (2014) Fatty acid-binding protein 4 (FABP4): pathophysiological insights and potent clinical biomarker of metabolic and cardiovascular diseases. Clin Med Insights Cardiol 8(Suppl 3):23–33
Wang YT, Liu CH, Zhu HL (2016) Fatty acid binding protein (FABP) inhibitors: a patent review (2012-2015). Expert Opin Ther Pat 26(7):767–776
Hirotsu C, Haba-Rubio J, Togeiro SM, Marques-Vidal P, Drager LF, Vollenweider P, Waeber G, Bittencourt L, Tufik S, Heinzer R (2018) Obstructive sleep apnoea as a risk factor for incident metabolic syndrome: a joined Episono and Hypnolaus prospective cohorts study. Eur Respir J 52:1801150
Huang T, Lin BM, Stampfer MJ, Tworoger SS, Hu FB, Redline SA (2018) Population-based study of the bidirectional association between obstructive sleep apnea and type 2 diabetes in three prospective U.S. cohorts. Diabetes Care 41(10):2111–2119
Ota H, Furuhashi M, Ishimura S, Koyama M, Okazaki Y, Mita T et al (2012) Elevation of fatty acid-binding protein 4 is predisposed by family history of hypertension and contributes to blood pressure elevation. Am J Hypertens 25(10):1124–1130
Yamada M, Mochizuki K, Honma K, Miyauchi R, Kasezawa N, Tohyama K et al (2015) Serum fatty acid binding protein 4 concentrations are positively and independently associated with blood pressure and abdominal fat among parameters in health check-ups in ordinary middle-aged Japanese males. J Nutr Sci Vitaminol 61(4):291–298
Furuhashi M, Mita T, Moniwa N, Hoshina K, Ishimura S, Fuseya T et al (2015) Angiotensin II receptor blockers decrease serum concentration of fatty acid-binding protein 4 in patients with hypertension. Hypertension Res 38(4):252–259
Lam JC, Xu A, Tam S, Khong PI, Yao TJ, Lam DC et al (2008) Hypoadiponectinemia is related to sympathetic activation and severity of obstructive sleep apnea. Sleep 31(12):1721–1727
Chen LD, Liu JN, Lin L, Wu Z, Li H, Ye YM et al (2015) Effect of continuous positive airway pressure on adiponectin in patients with obstructive sleep apnea: a meta-analysis. PloS One 10(9):e0136837
Recoquillon S, Pepin JL, Vielle B, Andriantsitohaina R, Bironneau V, Chouet-Girard F et al (2019) Effect of mandibular advancement therapy on inflammatory and metabolic biomarkers in patients with severe obstructive sleep apnoea: a randomised controlled trial. Thorax 74:496-499
Guo Y, Pan L, Ren D, Xie X (2013) Impact of continuous positive airway pressure on C-reactive protein in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath 17(2):495–503
Thunstrom E, Glantz H, Yucel-Lindberg T, Lindberg K, Saygin M, Peker Y (2017) CPAP does not reduce inflammatory biomarkers in patients with coronary artery disease and nonsleepy obstructive sleep apnea: a randomized controlled trial. Sleep. 40(11)
Alonso-Fernandez A, Garcia-Rio F, Arias MA, Hernanz A, de la Pena M, Pierola J, Barcelo A, Lopez-Collazo E, Agusti A (2009) Effects of CPAP on oxidative stress and nitrate efficiency in sleep apnoea: a randomised trial. Thorax. 64(7):581–586
Sivam S, Witting PK, Hoyos CM, Maw AM, Yee BJ, Grunstein RR, Phillips CL (2015) Effects of 8 weeks of CPAP on lipid-based oxidative markers in obstructive sleep apnea: a randomized trial. J Sleep Res 24(3):339–345
Stradling JR, Schwarz EI, Schlatzer C, Manuel AR, Lee R, Antoniades C et al (2015) Biomarkers of oxidative stress following continuous positive airway pressure withdrawal: data from two randomised trials. Eur Respir J 46(4):1065–1071
Acknowledgments
The authors would like to thank Ms. Choi Siu-Ling and all the staff in a sleep laboratory for coordination of investigations, Mr. Kelvin Lau for project coordination and data entry, and Ms. Michelle Cheong for manual scoring of polysomnogram.
Funding
The study was funded by the Research Grants Council of Hong Kong (grant number: 766707). The funding source had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research protocol was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster with HKW IRB reference number: UW07-178 and have been performed in accordance with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lui, M.M.S., Mak, J.C.W., Chong, P.W.C. et al. Circulating adipocyte fatty acid–binding protein is reduced by continuous positive airway pressure treatment for obstructive sleep apnea—a randomized controlled study. Sleep Breath 24, 817–824 (2020). https://doi.org/10.1007/s11325-019-01893-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01893-5