Abstract
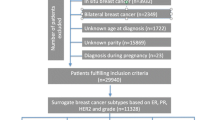
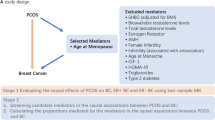
While childbearing protects against risk of epithelial ovarian cancer (EOC), few studies have explored the impact on maternal EOC risk of sex of offspring, which may affect the maternal environment during pregnancy. We performed a pooled analysis among parous participants from 12 case–controls studies comprising 6872 EOC patients and 9101 controls. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using multivariable logistic regression for case–control associations and polytomous logistic regression for histotype-specific associations, all adjusted for potential confounders. In general, no associations were found between offspring sex and EOC risk. However, compared to bearing only female offspring, bearing one or more male offspring was associated with increased risk of mucinous EOC (OR = 1.45; 95% CI = 1.01-2.07), which appeared to be limited to women reporting menarche before age 13 compared to later menarche (OR = 1.71 vs 0.99; P-interaction = 0.02). Bearing increasing numbers of male offspring was associated with greater risks of mucinous tumors (OR = 1.31, 1.84, 2.31, for 1, 2 and 3 or more male offspring, respectively; trend-p = 0.005). Stratifying by hormonally-associated conditions suggested that compared to bearing all female offspring, bearing a male offspring was associated with lower risk of endometrioid cancer among women with a history of adult acne, hirsutism, or polycystic ovary syndrome (OR = 0.49, 95% CI = 0.28-0.83) but with higher risk among women without any of those conditions (OR = 1.64 95% CI = 1.14–2.34; P-interaction = 0.003). Offspring sex influences the childbearing-EOC risk relationship for specific histotypes and conditions. These findings support the differing etiologic origins of EOC histotypes and highlight the importance of EOC histotype-specific epidemiologic studies. These findings also suggest the need to better understand how pregnancy affects EOC risk

Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, et al. SEER cancer statistics Review, 1975–2014, National Cancer Institute, Bethesda. https://seercancergov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017.
Moyer VA. Screening for ovarian cancer US Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2012;157(12):900–4.
Modugno F, Edwards RP. Ovarian cancer: prevention, detection, and treatment of the disease and its recurrence. Molecular mechanisms and personalized medicine meeting repor. Int J Gynecol Cancer. 2012;22(8):S45–57.
Cho KR, Shih Ie M. Ovarian cancer. Annu Rev Pathol. 2009;4:287–313.
Sung HK, Ma SH, Choi JY, Hwang Y, Ahn C, Kim BG, et al. The Effect of Breastfeeding Duration and Parity on the Risk of Epithelial Ovarian Cancer: a Systematic Review and Meta-analysis. J Prev Med Public Health. 2016;49(6):349–66.
Gaitskell K, Green J, Pirie K, Barnes I, Hermon C, Reeves GK, et al. Histological subtypes of ovarian cancer associated with parity and breastfeeding in the prospective Million Women Study. Int J Cancer. 2018;142(2):281–9.
Wentzensen N, Poole EM, Trabert B, White E, Arslan AA, Patel AV, et al. Ovarian Cancer Risk Factors by Histologic Subtype: an Analysis From the Ovarian Cancer Cohort Consortium. J Clin Oncol. 2016;34(24):2888–98.
Fathalla MF. Incessant ovulation–a factor in ovarian neoplasia? Lancet. 1971;2(7716):163.
Risch HA, Weiss NS, Lyon JL, Daling JR, Liff JM. Events of reproductive life and the incidence of epithelial ovarian cancer. Am J Epidemiol. 1983;117(2):128–39.
Risch HA. Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. J Natl Cancer Inst. 1998;90(23):1774–86.
Ness RB, Cottreau C. Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst. 1999;91(17):1459–67.
Toriola AT, Grankvist K, Agborsangaya CB, Lukanova A, Lehtinen M, Surcel HM. Changes in pre-diagnostic serum C-reactive protein concentrations and ovarian cancer risk: a longitudinal study. Ann Oncol. 2011;22(8):1916–21.
Obiekwe BC, Chard T. Human chorionic gonadotropin levels in maternal blood in late pregnancy: relation to birthweight, sex and condition of the infant at birth. Br J Obstet Gynaecol. 1982;89(7):543–6.
Adamcova K, Kolatorova L, Skodova T, Simkova M, Parizek A, Starka L, et al. Steroid hormone levels in the peripartum period—differences caused by fetal sex and delivery type. Physl Res. 2018;67:S489–97 Supplementum 3.
Boroditsky RS, Reyes FI, Winter JS, Faiman C. Serum human chorionic gonadotropin and progesterone patterns in the last trimester of pregnancy: relationship to fetal sex. Am J Obstet Gynecol. 1975;121(2):238–41.
Enninga EA, Nevala WK, Creedon DJ, Markovic SN, Holtan SG. Fetal sex-based differences in maternal hormones, angiogenic factors, and immune mediators during pregnancy and the postpartum period. Am J Reprod Immunol. 2015;73(3):251–62.
Toriola AT, Vaarasmaki M, Lehtinen M, Zeleniuch-Jacquotte A, Lundin E, Rodgers KG, et al. Determinants of maternal sex steroids during the first half of pregnancy. Obstet Gynecol. 2011;118(5):1029–36.
Steier JA, Ulstein M, Myking OL. Human chorionic gonadotropin and testosterone in normal and preeclamptic pregnancies in relation to fetal sex. Obstet Gynecol. 2002;100(3):552–6.
Ose J, Poole EM, Schock H, Lehtinen M, Arslan AA, Zeleniuch-Jacquotte A, et al. Androgens Are differentially associated with ovarian cancer subtypes in the ovarian cancer cohort consortium. Cancer Res. 2017;77(14):3951–60.
Trabert B, Michels KA, Anderson GL, Brinton LA, Falk RT, Geczik AM, et al. Circulating androgens and postmenopausal ovarian cancer risk in the Women’s Health Initiative Observational Study. Int J Cancer. 2019;145(8):2051–60.
Clifton VL, Murphy VE. Maternal asthma as a model for examining fetal sex-specific effects on maternal physiology and placental mechanisms that regulate human fetal growth. Placenta. 2004;25(Suppl A):S45–52.
Stark MJ, Dierkx L, Clifton VL, Wright IM. Alterations in the maternal peripheral microvascular response in pregnancies complicated by preeclampsia and the impact of fetal sex. J Soc Gynecol Investig. 2006;13(8):573–8.
Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–8.
Ying W, Catov JM, Ouyang P. Hypertensive Disorders of Pregnancy and Future Maternal Cardiovascular Risk. J Am Heart Assoc. 2018;7(17):e009382.
Gierach GL, Modugno F, Ness RB. Gender of offspring and maternal ovarian cancer risk. Gynecol Oncol. 2006;101(3):476–80.
Baik I, Lambe M, Liu Q, Cnattingius S, Mucci LA, Riman T, et al. Gender of offspring and maternal risk of invasive epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2007;16(11):2314–20.
Albrektsen G, Heuch I, Thoresen S, Kvale G. Twin births, sex of children and maternal risk of ovarian cancer: a cohort study in Norway. Br J Cancer. 2007;96(9):1433–5.
Jordan SJ, Green AC, Nagle CM, Olsen CM, Whiteman DC, Webb PM, et al. Beyond parity: association of ovarian cancer with length of gestation and offspring characteristics. Am J Epidemiol. 2009;170(5):607–14.
Fu Z, Moysich K, Ness RB, Modugno F. Gender of offspring and risk of ovarian cancer: the HOPE study. Cancer Epidemiol. 2019;64:101646.
Committee on the State of the Science in Ovarian Cancer R, Board on Health Care S, Institute of M, National Academies of Sciences E, Medicine. Ovarian Cancers: Evolving Paradigms in Research and Care. Washington (DC): National Academies Press (US) Copyright 2016 by the National Academy of Sciences. All rights reserved; 2016.
Ramus SJ, Vierkant RA, Johnatty SE, Pike MC, Van Den Berg DJ, Wu AH, et al. Consortium analysis of 7 candidate SNPs for ovarian cancer. Int J Cancer. 2008;123(2):380–8.
Merritt MA, Green AC, Nagle CM, Webb PM. Talcum powder, chronic pelvic inflammation and NSAIDs in relation to risk of epithelial ovarian cancer. Int J Cancer. 2008;122(1):170–6.
Risch HA, Bale AE, Beck PA, Zheng W. PGR +331 A/G and increased risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2006;15(9):1738–41.
Royar J, Becher H, Chang-Claude J. Low-dose oral contraceptives: protective effect on ovarian cancer risk. Int J Cancer. 2001;95(6):370–4.
Goodman MT, Lurie G, Thompson PJ, McDuffie KE, Carney ME. Association of two common single-nucleotide polymorphisms in the CYP19A1 locus and ovarian cancer risk. Endocr Relat Cancer. 2008;15(4):1055–60.
Lo-Ciganic WH, Zgibor JC, Bunker CH, Moysich KB, Edwards RP, Ness RB. Aspirin, nonaspirin nonsteroidal anti-inflammatory drugs, or acetaminophen and risk of ovarian cancer. Epidemiology. 2012;23(2):311–9.
Lurie G, Wilkens LR, Thompson PJ, McDuffie KE, Carney ME, Terada KY, et al. Combined oral contraceptive use and epithelial ovarian cancer risk: time-related effects. Epidemiology. 2008;19(2):237–43.
Schildkraut JM, Iversen ES, Wilson MA, Clyde MA, Moorman PG, Palmieri RT, et al. Association between DNA damage response and repair genes and risk of invasive serous ovarian cancer. PLoS ONE. 2010;5(4):e10061.
Bandera EV, King M, Chandran U, Paddock LE, Rodriguez-Rodriguez L, Olson SH. Phytoestrogen consumption from foods and supplements and epithelial ovarian cancer risk: a population-based case control study. BMC Womens Health. 2011;11:40.
Risch HA, Marrett LD, Howe GR. Parity, contraception, infertility, and the risk of epithelial ovarian cancer. Am J Epidemiol. 1994;140(7):585–97.
Pal T, Permuth-Wey J, Betts JA, Krischer JP, Fiorica J, Arango H, et al. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer. 2005;104(12):2807–16.
Balogun N, Gentry-Maharaj A, Wozniak EL, Lim A, Ryan A, Ramus SJ, et al. Recruitment of newly diagnosed ovarian cancer patients proved challenging in a multicentre biobanking study. J Clin Epidemiol. 2011;64(5):525–30.
Ness RB, Cramer DW, Goodman MT, Kjaer SK, Mallin K, Mosgaard BJ, et al. Infertility, fertility drugs, and ovarian cancer: a pooled analysis of case–control studies. Am J Epidemiol. 2002;155(3):217–24.
Wu AH, Pearce CL, Tseng CC, Templeman C, Pike MC. Markers of inflammation and risk of ovarian cancer in Los Angeles County. Int J Cancer. 2009;124(6):1409–15.
Olsen CM, Nagle CM, Whiteman DC, Ness R, Pearce CL, Pike MC, et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr Relat Cancer. 2013;20(2):251–62.
Chen P, Wang DB, Liang YM. Evaluation of estrogen in endometriosis patients: regulation of GATA-3 in endometrial cells and effects on Th2 cytokines. J Obstet Gynaecol Res. 2016;42(6):669–77.
Al-Sabbagh M, Lam EW, Brosens JJ. Mechanisms of endometrial progesterone resistance. Mol Cell Endocrinol. 2012;358(2):208–15.
Nisenblat V, Norman RJ. Androgens and polycystic ovary syndrome. Curr Opin Endocrinol Diabetes Obes. 2009;16(3):224–31.
Diamanti-Kandarakis E. Polycystic ovarian syndrome: pathophysiology, molecular aspects and clinical implications. Expert Rev Mol Med. 2008;10:e3.
Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E. American association of clinical endocrinologists, Amercian college of endocrinology, and androgen excess and PCOS society disease state clinical review: guide to the best practices in the evaluation and treament of polycystic syndrome – part 1. Endocr Pract. 2015;21(11):1291–300.
Apter D, Vihko R. Early menarche, a risk factor for breast cancer, indicates early onset of ovulatory cycles. J Clin Endocrinol Metab. 1983;57(1):82–6.
Vihko R, Apter D. Endocrine characteristics of adolescent menstrual cycles: impact of early menarche. J Steroid Biochem. 1984;20(1):231–6.
Bernstein L, Pike MC, Ross RK, Henderson BE. Age at menarche and estrogen concentrations of adult women. Cancer Causes Control. 1991;2(4):221–5.
Kopelman PG. Hormones and obesity. Baillieres Clin Endocrinol Metab. 1994;8(3):549–75.
Pasquali R. Obesity and androgens: facts and perspectives. Fertil Steril. 2006;85(5):1319–40.
Rosenfield RL. Clinical review: adolescent anovulation: maturational mechanisms and implications. J Clin Endocrinol Metab. 2013;98(9):3572–83.
Gaspard UJ, Romus MA, Gillain D, Duvivier J, Demey-Ponsart E, Franchimont P. Plasma hormone levels in women receiving new oral contraceptives containing ethinyl estradiol plus levonorgestrel or desogestrel. Contraception. 1983;27(6):577–90.
Brenner PF, Mishell DR Jr, Stanczyk FZ, Goebelsmann U. Serum levels of d-norgestrel, luteinizing hormone, follicle-stimulating hormone, estradiol, and progesterone in women during and following ingestion of combination oral contraceptives containing dl-norgestrel. Am J Obstet Gynecol. 1977;129(2):133–40.
Mishell DR Jr, Thorneycroft IH, Nakamura RM, Nagata Y, Stone SC. Serum estradiol in women ingesting combination oral contraceptive steroids. Am J Obstet Gynecol. 1972;114(7):923–8.
Baron JA, La Vecchia C, Levi F. The antiestrogenic effect of cigarette smoking in women. Am J Obstet Gynecol. 1990;162(2):502–14.
Cramer DW, Welch WR. Determinants of ovarian cancer risk. II. Inferences regarding pathogenesis. J Natl Cancer Inst. 1983;71(4):717–21.
Zeitlin J, Saurel-Cubizolles MJ, De Mouzon J, Rivera L, Ancel PY, Blondel B, et al. Fetal sex and preterm birth: are males at greater risk? Hum Reprod. 2002;17(10):2762–8.
Di Renzo GC, Rosati A, Sarti RD, Cruciani L, Cutuli AM. Does fetal sex affect pregnancy outcome? Gend Med. 2007;4(1):19–30.
Retnakaran R, Kramer CK, Ye C, Kew S, Hanley AJ, Connelly PW, et al. Fetal sex and maternal risk of gestational diabetes mellitus: the impact of having a boy. Diab Care. 2015;38(5):844–51.
Shiozaki A, Matsuda Y, Satoh S, Saito S. Impact of fetal sex in pregnancy-induced hypertension and preeclampsia in Japan. J Reprod Immunol. 2011;89(2):133–9.
Clifton V. Maternal asthma during pregnancy and fetal outcomes: potential mechanisms and possible solutions. Curr Opin Allergy Clin Immunol. 2006;6(5):307–11.
Gong S, Sovio U, Aye IL, Gaccioli F, Dopierala J, Johnson MD, et al. Placental polyamine metabolism differs by fetal sex, fetal growth restriction, and preeclampsia. JCI Insight. 2018;3(13):e120723.
Nelson JL. Microchimerism and human autoimmune diseases. Lupus. 2002;11(10):651–4.
Gammill HS, Nelson JL. Naturally acquired microchimerism. Int J Dev Biol. 2010;54(2–3):531–43.
Bianchi DW, Zickwolf GK, Weil GJ, Sylvester S, DeMaria MA. Male fetal progenitor cells persist in maternal blood for as long as 27 years postpartum. Proc Natl Acad Sci U S A. 1996;93(2):705–8.
Hallum S, Jakobsen MA, Gerds TA, Pinborg A, Tjønneland A, Kamper-Jørgensen M. Male origin microchimerism and ovarian cancer. Int J Epidemiol 2020. https://doi.org/10.1093/ije/dyaa019.
Seidman JD, Kurman RJ, Ronnett BM. Primary and metastatic mucinous adenocarcinomas in the ovaries: incidence in routine practice with a new approach to improve intraoperative diagnosis. Am J Surg Pathol. 2003;27(7):985–93.
Risch HA, Marrett LD, Jain M, Howe GR. Differences in risk factors for epithelial ovarian cancer by histologic type. Results of a case-control study. Am J Epidemiol. 1996;144(4):363–72.
Yang HP, Murphy KR, Pfeiffer RM, George N, Garcia-Closas M, Lissowska J, et al. Lifetime Number of Ovulatory Cycles and Risks of Ovarian and Endometrial Cancer Among Postmenopausal Women. Am J Epidemiol. 2016;183(9):800–14.
Webb PM, Green A, Cummings MC, Purdie DM, Walsh MD, Chenevix-Trench G. Relationship between number of ovulatory cycles and accumulation of mutant p53 in epithelial ovarian cancer. J Natl Cancer Inst. 1998;90(22):1729–34.
Trabert B, Tworoger SS, O’Brien KM, Townsend MK, Fortner RT, Iversen ES, et al. The Risk of Ovarian Cancer Increases with an Increase in the Lifetime Number of Ovulatory Cycles: an Analysis from the Ovarian Cancer Cohort Consortium (OC3). Cancer Res. 2020;80(5):1210–8.
Lee AW, Ness RB, Roman LD, Terry KL, Schildkraut JM, Chang-Claude J, et al. association between menopausal estrogen-only therapy and ovarian carcinoma risk. Obstet Gynecol. 2016;127(5):828–36.
Beral V, Gaitskell K, Hermon C, Moser K, Reeves G, Peto R. Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies. Lancet. 2015;385(9980):1835–42.
Pearce CL, Templeman C, Rossing MA, Lee A, Near AM, Webb PM, et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case–control studies. Lancet Oncol. 2012;13(4):385–94.
Kurman RJ, Shih Ie M. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer–shifting the paradigm. Hum Pathol. 2011;42(7):918–31.
Jarboe EA, Folkins AK, Drapkin R, Ince TA, Agoston ES, Crum CP. Tubal and ovarian pathways to pelvic epithelial cancer: a pathological perspective. Histopathology. 2009;55(5):619.
Acknowledgements
We are grateful to the family and friends of Kathryn Sladek Smith for their generous support of the Ovarian Cancer Association Consortium through their donations to the Ovarian Cancer Research Fund. We thank the study participants, doctors, nurses, research staff, clinical and scientific collaborators, health care providers, and health information sources who have contributed to the many studies contributing to this manuscript. Acknowledgements for individual studies: AUS: The AOCS also acknowledges the cooperation of the participating institutions in Australia, and the contribution of the study nurses, research assistants and all clinical and scientific collaborators. The complete AOCS Study Group can be found at www.aocstudy.org. We would like to thank all of the women who participated in this research program; CON: The cooperation of the 32 Connecticut hospitals, including Stamford Hospital, in allowing patient access, is gratefully acknowledged. This study was approved by the State of Connecticut Department of Public Health Human Investigation Committee. Certain data used in this study were obtained from the Connecticut Tumor Registry in the Connecticut Department of Public Health. The authors assume full responsibility for analyses and interpretation of these data; GER: The German Ovarian Cancer Study (GER) thank Sabine Behrens for competent technical assistance; UKO: We particularly thank I. Jacobs, M. Widschwendter, E. Wozniak, A. Ryan, J. Ford and N. Balogun for their contribution to the study.
Funding
The Ovarian Cancer Association Consortium was supported by a grant from the Ovarian Cancer Research Fund thanks to donations by the family and friends of Kathryn Sladek Smith (PPD/RPCI.07). Funding for individual studies: AUS: The Australian Ovarian Cancer Study (AOCS) was supported by the U.S. Army Medical Research and Materiel Command (DAMD17-01-1-0729), National Health & Medical Research Council of Australia (199600, 400413 and 400281), Cancer Councils of New South Wales, Victoria, Queensland, South Australia and Tasmania and Cancer Foundation of Western Australia (Multi-State Applications 191, 211 and 182). AOCS gratefully acknowledges additional support from Ovarian Cancer Australia and the Peter MacCallum Foundation; CON: National Institutes of Health (R01-CA074850; R01-CA080742); DKE: Ovarian Cancer Research Fund; GER: German Federal Ministry of Education and Research, Programme of Clinical Biomedical Research (01 GB 9401) and the German Cancer Research Center (DKFZ); HAW: U.S. National Institutes of Health (R01-CA58598, N01-CN-55424 and N01-PC-67001); HOP: University of Pittsburgh School of Medicine Dean’s Faculty Advancement Award (F. Modugno), Department of Defense (DAMD17-02-1-0669) and NCI (K07-CA080668, R01-CA95023, MO1-RR000056 R01-CA126841); NCO: National Institutes of Health (R01-CA76016) and the Department of Defense (DAMD17-02-1-0666); NJO: National Cancer Institute (NIH-K07 CA095666, R01-CA83918, NIH-K22-CA138563, and P30-CA072720) and Rutgers Cancer Institute of New Jersey; SON: National Health Research and Development Program, Health Canada, grant 6613-1415-53; TBO: National Institutes of Health (R01-CA106414-A2), American Cancer Society (CRTG-00-196-01-CCE), Department of Defense (DAMD17-98-1-8659), Celma Mastery Ovarian Cancer Foundation; TOR: NIH grants R01 CA063678 and R01 CA063682; UKO: The UKOPS study was funded by The Eve Appeal (The Oak Foundation) with investigators supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre and MRC core funding (MR_UU_12023); USC: P01CA17054, P30CA14089, R01CA61132, N01PC67010, R03CA113148, R03CA115195, N01CN025403, and California Cancer Research Program (00-01389 V-20170, 2II0200).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Usha Menon has stock ownership awarded to her by UCL in Abcodia. No other authors report conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Modugno, F., Fu, Z., Jordan, S.J. et al. Offspring sex and risk of epithelial ovarian cancer: a multinational pooled analysis of 12 case–control studies. Eur J Epidemiol 35, 1025–1042 (2020). https://doi.org/10.1007/s10654-020-00682-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-020-00682-9