Abstract
Background
Preterm premature rupture of membrane (pPROM) leads to high neonatal mortality due in part to severe lung hypoplasia (LH). In other causes of severe LH, fetal echo-based parameters of smaller branch pulmonary arteries (PA), shorter acceleration to ejection time ratio (AT/ET), increased peak early diastolic reverse flow (PEDRF), and higher pulsatility index (PI) are predictive of worse neonatal outcome. We sought to determine whether these parameters correlated with worse clinical outcome in pPROM.
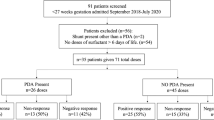
Methods
Twenty-five pregnancies complicated by pPROM were prospectively recruited. Fetal echocardiography was used to evaluate branch PA diameters and Doppler parameters. Clinical records were reviewed. Fetal echo findings were compared between early survivors and non-survivors.
Results
Of 25 pPROM cases, 5 had early neonatal demise (≤3 days) due to respiratory insufficiency. While gestational age at pPROM, fetal echo, and at birth did not differ, amniotic fluid index (AFI) was significantly lower in early non-survivors compared to survivors (p = 0.05). No difference was observed in PA diameter, PEDRF, or PI; however, branch PA AT/ET was significantly shorter in non-survivors (right PA median 0.12 (0.11–0.16) vs. survivors 0.17 (0.14–0.21), p = 0.046 and left PA 0.12 (0.09–0.13) vs. survivors 0.16 (0.11–0.21), p = 0.042).
Conclusions
We found a significantly lower AFI and shorter fetal bilateral branch PA AT/ET to be associated with early neonatal demise following pPROM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Winn HN, Chen M, Amon E, Leet TL, Shumway JB, Mostello D. Neonatal pulmonary hypoplasia and perinatal mortality in patients with midtrimester rupture of amniotic membranes-a critical analysis. Am J Obstet Gynecol. 2000;182:1638–44.
Laudy JA, Tibboel D, Robben SG, De Krijger RR, De Ridder MA, Wladimiroff JW. Prenatal prediction of pulmonary hypoplasia: clinical, biometric, and Doppler velocity correlates. Pediatrics. 2002;109:250–8.
Bohn D, Lacro RV, Ryan G, Stephens D, Rabinovitch M, Smallhorn JS, et al. Fetal pulmonary artery diameters and their association with lung hypoplasia and postnatal outcome in congenital diaphragmatic hernia. Am J Obstet Gynecol. 2002;186:1085–90.
Derderian SC, Jayme CM, Cheng LS, Keller RL, Moon-Grady AJ, Mackenzie TC. Mass effect alone may not explain pulmonary vascular pathology in severe congenital diaphragmatic hernia. Fetal Diagn Ther. 2016;39:117–24.
Yamamoto Y, Thebaud B, Vadivel A, Eaton F, Jain V, Hornberger LK. Doppler parameters of fetal lung hypoplasia and impact of sildenafil. Am J Obstet Gynecol. 2014;211:263.e1–8.
Fuke S, Kanaki T, Mu J, Wasada K, Takemura M, Mitsuda N, et al. Antenatal prediction of pulmonary hypoplasia by acceleration time/ejection time ratio of fetal pulmonary arteries by Doppler blood flow velocimetry. Am J Obstet Gynecol. 2003;188:228–33.
Moreno-Alvarez O, Hernandez-Andrade E, Oris D, Jani J, Deprest J, Gratacos E. Association between intrapulmonary arterial Doppler parameters and degree of lung growth as measured by lung-to-head ratio in fetuses with congenital diaphragmatic hernia. Ultrasound Obstet Gynecol. 2008;31:164–70.
Broth RE, Wood DC, Rasanen J, Sabogal J, Komwilaisak R, Weiner S, et al. Prenatal prediction of lethal pulmonary hypoplasia: the hyperoxygenation test for pulmonary artery reactivity. Am J Obstet Gynecol. 2002;187:940–5.
Rasanen J, Wood DC, Debbs RH, Cohen J, Weiner S, Huhta JC. Reactivity of the human fetal pulmonary circulation to maternal hyperoxygenation increases during the second half of pregnancy: a randomized study. Circulation. 1998;97:257–62.
Yamamoto Y, Hirose A, Howley L, Savard W, Jain V, Hornberger LK. Parameters of fetal pulmonary vascular health: baseline trends and response to maternal hyperoxia in the second and third trimesters. Ultrasound Obstet Gynecol. 2017;50:618–23.
Sokol J, Shimizu N, Bohn D, Doherty D, Ryan G, Hornberger LK. Fetal pulmonary artery diameter measurements as a predictor of morbidity in antenatally diagnosed congenital diaphragmatic hernia: a prospective study. Am J Obstet Gynecol. 2006;195:470–7.
Davidson LM, Berkelhamer SK. Bronchopulmonary dysplasia: chronic lung disease of infancy and long-term pulmonary outcomes. J Clin Med. 2017;6:1–20.
Schneider C, McCrindle BW, Carvahlo JS, Hornberger LK, McCarthy KP, Daubeney PE. Development of Z-scores for fetal cardiac dimensions from echocardiography. Ultrasound Obstet Gynecol. 2005;26:599–605.
Jani J, Nicolaides KH, Keller RL, Benachi A, Peralta CF, Favre R, et al. Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007;30:67–71.
Goncalves AN, Correia-Pinto J, Nogueira-Silva C. Imagiological methods for prediction of fetal pulmonary hypoplasia: a systematic review. J Matern Fetal Neonatal Med. 2019:1–10. https://doi.org/10.1080/14767058.2019.1636029.
Van Teeffelen AS, Van Der Heijden J, Oei SG, Porath MM, Willekes C, Opmeer B, et al. Accuracy of imaging parameters in the prediction of lethal pulmonary hypoplasia secondary to mid-trimester prelabor rupture of fetal membranes: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2012;39:495–9.
Katayama S, Tada K, Nakanishi Y, Takata M, Kumazawa K, Tsukahara S, et al. Evaluation of normal fetal branch pulmonary artery diameters measured by ultrasonography: a comparison with congenital diaphragmatic hernia. Fetal Diagn Ther. 2008;23:303–7.
Kitabatake A, Inoue M, Asao M, Masuyama T, Tanouchi J, Morita T, et al. Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique. Circulation. 1983;68:302–9.
Azpurua H, Norwitz ER, Campbell KH, Funai EF, Pettker CM, Kleine M, et al. Acceleration/ejection time ratio in the fetal pulmonary artery predicts fetal lung maturity. Am J Obstet Gynecol. 2010;203:40.e1–8.
Lorthe E, Ancel PY, Torchin H, Kaminski M, Langer B, Subtil D, et al. Impact of latency duration on the prognosis of preterm infants after preterm premature rupture of membranes at 24 to 32 weeks’ gestation: a national population-based cohort study. J Pediatr. 2017;182:47–52.e2.
Porter HJ. Pulmonary hypoplasia. Arch Dis Child Fetal Neonatal Ed. 1999;81:F81–3.
Thibeault DW, Kilbride HK. Increased acinar arterial wall muscle in preterm infants with PROM and pulmonary hypoplasia. Am J Perinatol. 1997;14:457–60.
Donahoe PK, Longoni M, High FA. Polygenic causes of congenital diaphragmatic hernia produce common lung pathologies. Am J Pathol. 2016;186:2532–43.
Acknowledgements
We want to thank to Takahisa Ogawa, MD, MPH, Harvard T.H. Chan School of Public Health, Department of Epidemiology, who helped our statistical analysis.
Author information
Authors and Affiliations
Contributions
AH and VJ recruited pPROM patients. YY, AH, and LKH performed the fetal echocardiograms and collected the fetal data. YY analyzed the data. YY and LKH generated the paper with input from AH and VJ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamamoto, Y., Hirose, A., Jain, V. et al. Branch pulmonary artery Doppler parameters predict early survival–non-survival in premature rupture of membranes. J Perinatol 40, 1821–1827 (2020). https://doi.org/10.1038/s41372-020-00817-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00817-6
This article is cited by
-
Polo-like kinase 1 promotes pulmonary hypertension
Respiratory Research (2023)