Abstract
Purpose
Invasive lobular carcinoma (ILC) is a distinct histological subtype of breast cancer that can make early detection with mammography challenging. We compared imaging performance of digital breast tomosynthesis (DBT) to digital mammography (DM) for diagnoses of ILC, invasive ductal carcinoma (IDC), and invasive mixed carcinoma (IMC) in a screening population.
Methods
We included screening exams (DM; n = 1,715,249 or DBT; n = 414,793) from 2011 to 2018 among 839,801 women in the Breast Cancer Surveillance Consortium. Examinations were followed for one year to ascertain incident ILC, IDC, or IMC. We measured cancer detection rate (CDR) and interval invasive cancer rate/1000 screening examinations for each histological subtype and stratified by breast density and modality. We calculated relative risk (RR) for DM vs. DBT using log-binomial models to adjust for the propensity of receiving DBT vs. DM.
Results
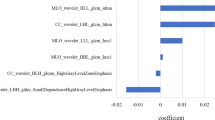
Unadjusted CDR per 1000 mammograms of ILC overall was 0.33 (95%CI: 0.30–0.36) for DM; 0.45 (95%CI: 0.39–0.52) for DBT, and for women with dense breasts- 0.33 (95%CI: 0.29–0.37) for DM and 0.54 (95%CI: 0.43–0.66) for DBT. Similar results were noted for IDC and IMC. Adjusted models showed a significantly increased RR for cancer detection with DBT compared to DM among women with dense breasts for all three histologies (RR; 95%CI: ILC 1.53; 1.09–2.14, IDC 1.21; 1.02–1.44, IMC 1.76; 1.30–2.38), but no significant increase among women with non-dense breasts.
Conclusion
DBT was associated with higher CDR for ILC, IDC, and IMC for women with dense breasts. Early detection of ILC with DBT may improve outcomes for this distinct clinical entity.
Similar content being viewed by others
Data availability
Data:: BCSC (bcsc-research.org). Data collected and maintained by the Breast Cancer Surveillance Consortium are protected by a Federal Certificate of Confidentiality from the National Institutes of Health (NIH). Per the terms of this certificate, identifiable data shall be disclosed only when: required by federal, state, or local laws; necessary for medical treatment of the individual to whom the data pertains; made with the consent of the individual; or made for the purposes of other scientific research complying with federal regulations governing human subjects research. For more details on these protections and their limits, please visit the NIH Certificate of Confidentiality Website.
References
Mouabbi JA, Hassan A, Lim B et al (2022) Invasive lobular carcinoma: an understudied emergent subtype of breast cancer. Breast Cancer Res Treat 193:253–264
Johnson K, Sarma D, Hwang ES (2015) Lobular breast cancer series: imaging. Breast Cancer Res 17:94
Porter AJ, Evans EB, Foxcroft LM et al (2013) Mammographic and ultrasound features of invasive lobular carcinoma of the breast. J Med Imag Rad Oncol 5(1):1–10
McCart Reed AE, Kalinowski L, Simpson PT et al (2021) Invasive lobular carcinoma of the breast: the increasing importance of this special subtype. Breast Cancer Res Treat 23:6. https://doi.org/10.1186/s13058-020-01384-6
Romanucci G, Zantedeschi L, Ventriglia A et al (2021) Lobular breast cancer conspicuity on digital breast tomosynthesis compared to synthesized 2D mammography: a multireader study. J Imag 7(9):185. https://doi.org/10.3390/jimaging7090185
McDonald ES, Oustimov A, Weinstein SP et al (2016) Effectiveness of digital breast tomosynthesis compared with digital mammography: outcomes analysis from 3 years of breast cancer screening. JAMA Oncol 2(6):737–743. https://doi.org/10.1001/jamaoncol.2015.5536
Alabousi M, Wadera A, Kashif Al-Ghita M et al (2021) Performance of digital breast tomosynthesis, synthetic f¢mammography, and digital mammography in breast cancer screening: a systematic review and meta-analysis. J Nat Cancer Institute 113(6):680–690
Lowry KP, Coley RY, Miglioretti DL et al (2021) Screening performance of digital breast tomosynthesis vs digital mammography in community practice by patient age, screening round, and breast density. JAMA Netw Open 3(7):e2011792–e2011792
Kerlikowske K, Su Y, Sprague BL et al (2022) Association of screening with digital breast tomosynthesis vs digital mammography with risk of interval invasive and advanced breast cancer. JAMA 327(22):2220–2230. https://doi.org/10.1001/jama.2022.7672
Menezes GLG, van den Bosch MAAJ, Postma EL et al (2013) Invasive ductolobular carcinoma of the breast: spectrum of mammographic, ultrasound and magnetic resonance imaging findings correlated with proportion of the lobular component. Springerplus 2:621
Chammings F, Kao E, Ladis A et al (2017) Imagine features and conspicuity of invasive lobular carcinomas on digital breast tomosynthesis. Br J Radiol 90:20170128
Grubstein A, Rapson Y, Morgenstern S et al (2016) Invasive lobular carcinoma of the breast: appearance on digital breast tomosynthesis. Breast Care 11:359–362
Mariscotti G, Durando M, Houssami N et al (2016) Digital breast tomosynthesis as an adjunct to digital mammography for detecting and characterising invasive lobular cancers: a multi-reader study. Clin Radiol 71(9):889–895
Yun SJ, Ryu CW, Rhee SJ et al (2017) Benefit of adding digital breast tomosynthesis to digital mammography for breast cancer screening focused on cancer characteristics: a meta-analysis. Breast Cancer Res Treat 164:557–569
Fuji MH, Herschorn SD, Sowden M et al (2019) Detection rates for benign and malignant diagnoses on breast cancer screening with digital breast tomosynthesis in a statewide mammography registry study. AJR Am J Roentgenol 212(3):706
Breast Cancer Surveillance Consortium. About the BCSC :: BCSC (bcsc-research.org). Last Accessed: 7/31/2022.
Breast Cancer Surveillance Consortium. Standard Definitions :: BCSC (bcsc-research.org). Last Accessed: 7/31/2022.
Arpino G, Bardou VJ, Clark GM, et al. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 2004;6(3):R149–56. Da Ros L, Moretti A, Querzoli P, et al. HER2-positive lobular versus ductal carcinoma of the breast: pattern of first recurrence and molecular insights. Clin Breast Cancer. 2018;18(5):e1133–9.
Christgen M, Gluz O, Harbeck N et al (2020) Differential impact of prognostic parameters in hormone receptor-positive lobular breast cancer. Cancer 126(22):4847–4858
Flores-Diaz D, Arce C, Flores-Luna L et al (2019) Impact of invasive lobular carcinoma on long-term outcomes in Mexican breast cancer patients. Breast Cancer Res Treat 176(1):243–249
Altundag K (2019) HER2+ and triple-negative phenotypes in invasive lobular carcinoma might have different specific biological features. Breast Cancer Res Treat 176(3):719
Turner NC, Slamon DJ, Ro J et al (2018) Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med 379(20):1926–1936
Palbociclib and Endocrine Therapy for LObular Breast Cancer Preoperative Study (PELOPS) United states: National library of Medicine; 2016 [Available from: https://clinicaltrials.gov/ct2/show/NCT0276454. Accessed Oct 2020.
Assessing Efficacy of Carboplatin and ATezOlizumab in Metastatic Lobular Breast Cancer (GELATO) Netherlands2017 Available from: https://clinicaltrials.gov/ct2/show/NCT03147040. Accessed Oct 2020.
ROS1 Targeting With Crizotinib in Advanced E-cadherin Negative, ER Positive Lobular Breast Cancer or Diffuse Gastric Cancer Study (ROLo) United Kingdom2019 [Available from: https://clinicaltrials.gov/ct2/show/NCT0362064. Accessed Oct 2020.
Neoadjuvant Study of Targeting ROS1 in Combination With Endocrine Therapy in Invasive Lobular Carcinoma of the Breast (ROSALINE) [available from https://clinicaltrials.gov/ct2/show/NCT04551495]. Accessed Oct 2020.
Perez-Garcia J, Cortes J, Metzger-Filho O (2019) Efficacy of single-agent chemotherapy for patients with advanced invasive lobular carcinoma: a pooled analysis from three clinical trials. Oncologist 24(8):1041–1047
Ruhstaller T, Giobbie-Hurder A, Colleoni M et al (2019) Adjuvant letrozole and tamoxifen alone or sequentially for postmenopausal women with hormone receptor-positive breast cancer: long-term follow-up of the BIG 1–98 trial. J Clin Oncol 37(2):105–114
Metzger-Filho O, Ferreira AR, Jeselsohn R et al (2019) Mixed invasive ductal and lobular carcinoma of the breast: prognosis and the importance of histologic grade. Oncologist 24(7):e441–e449. https://doi.org/10.1634/theoncologist.2018-0363
Hogan MP, Amir T, Sevilimedu V et al (2021) AJR Am J Roentgenol 216(6):1486–1491. https://doi.org/10.2214/AJR.20.23480
Acknowledgements
The collection of cancer and vital status data used in this study was supported in part by several state public health departments and cancer registries throughout the U.S. For a full description of these sources, please see: https://www.bcsc-research.org/about/work-acknowledgement. All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee, nor those of the National Cancer Institute or the National Institutes of Health. We thank the participating women, mammography facilities, and radiologists for the data they have provided for this study. You can learn more about the BCSC at: http://www.bcsc-research.org/.
The collection of cancer incidence and vital status data used in this study was supported, in part, by:
The California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Sect. 103,885; the National Cancer Institute's Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement U58-DP003862-01 awarded to the California Department of Public Health;
The Vermont Cancer Registry, supported in part by Cooperative Agreement NU58DP006322 from the Centers for Disease Control and Prevention, awarded to the Vermont State Agency of Human Services.
The Cancer Surveillance System of the Fred Hutchinson Cancer Research Center, which is funded by contracts N01-CN-005230, N01-CN-67009, N01-PC-35142, HHSN261201000029C, and HHSN261201300012I from the Surveillance, Epidemiology and End Results (SEER) Program of the National Cancer Institute with additional support from the Fred Hutchinson Cancer Research Center and the State of Washington;
The New Hampshire State Cancer Registry supported in part by cooperative agreement U55/CCU-121912 awarded to the New Hampshire Department of Health and Human Services, Division of Public Health Services, Bureau of Disease Control and Health Statistics, Health Statistics and Data Management Section;
The North Carolina Central Cancer Registry, which is partially supported by the Centers for Disease Control and Prevention under cooperative agreement DP12-120503CONT14;
Manuscripts including data from the Metro Chicago Breast Cancer Registry were supported in part by the Illinois Department of Public Health, Illinois State Cancer Registry which is partially supported by the Centers for Disease Control and Prevention under cooperative agreement DP12-120504CONT15.
The ideas and opinions expressed herein are those of the authors and endorsement by the State of California, the California Department of Public Health; Illinois Department of Public Health; New Hampshire Department of Health and Human Services; the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
We thank the participating women, mammography facilities, and radiologists for the data they have provided for this study.
Funding
This work was supported by the Breast Cancer Surveillance Consortium with funding from the National Cancer Institute (P01CA154292, U54CA163303, R01CA149365, R50CA211115) and the Agency for Health Research and Quality (R01 HS018366-01A1). Data collection for this research was additionally funded through a Patient-Centered Outcomes Research Institute (PCORI) Program Award (PCS-1504–30370).
Author information
Authors and Affiliations
Contributions
Conceptualization: TO, DLM, CIL, RMD; Data curation: TO, LA, DLM, CIL, LMH, KK, DW, BLS, EJAB; Formal Analysis: LA, TO, DLM. Methodology: TO, LA, DLM, CIL, LMH, KK, DW, BLS, EJAB, RMD. Supervision: TO. Writing—original draft: TO. Writing—review & editing: TO, LA, DLM, CIL, LMH, KK, DW, BLS, EJAB, RMD. The National Cancer Institute had no role in the study’s design; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication. Likewise, the content in this manuscript is solely the responsibility of the authors and does not necessarily represent the views of PCORI, its Board of Governors or Methodology Committee.
Corresponding author
Ethics declarations
Conflict of interest
C.I. Lee receives personal fees from the American College of Radiology for journal editorial board work and textbook royalties from UpToDate, Inc., Oxford University Press, and McGraw Hill, Inc. There are no other conflicts of interest to disclosure for any of the other authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Onega, T., Abraham, L., Miglioretti, D.L. et al. Digital mammography and digital breast tomosynthesis for detecting invasive lobular and ductal carcinoma. Breast Cancer Res Treat 202, 505–514 (2023). https://doi.org/10.1007/s10549-023-07051-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07051-6