Abstract
Background
Moyamoya disease and atherosclerotic cerebrovascular occlusive disease lead to hemodynamic impairment of cerebral blood flow. One major differentiation between both disease entities lies in the collateralization pathways. The clinical implications of the collateralization pathways for the development of hemodynamic ischemia remain unknown. The aim was to characterize collateralization and ischemia patterns in patients with chronic hemodynamic compromise.
Methods
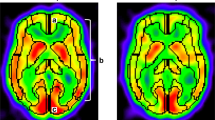
Hemodynamic compromise was verified using acetazolamide-stimulated xenon-CT or SPECT in 54 patients [30 moyamoya and 24 atherosclerotic cerebrovascular disease (ACVD)]. All patients received MRI to differentiate hemodynamic ischemia into anterior/posterior cortical border zone infarction (CBI), inferior border zone infarction (IBI) or territorial infarction (TI). Digital subtraction angiography was applied to evaluate collateralization. Collateralization was compared and correlated with the localization of ischemia and number of vascular territories with impaired cerebrovascular reserve capacity (CVRC).
Results
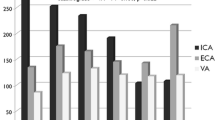
MM patients showed collateralization significantly more often via pericallosal anastomosis and the posterior communicating artery (flow in the anterior-posterior direction; MM: 95 %/95 % vs. ACVD: 23 %/12 %, p < 0.05). ACVD patients demonstrated collateralization via the anterior and posterior communicating arteries (flow in the posterior-anterior direction, MM: 6 %/5 % vs. ACVD: 62 %/88 %, p < 0.05). Patterns of infarction were comparable (aCBI: MM: 36 % vs. ACVD: 35 %; pCBI: MM: 10 % vs. ACVD: 20 %; IBI: MM: 35 % vs. ACVD: 41 %; TI: MM: 13 % vs. ACVD: 18 %). The number and localization of vascular territories with impaired CVRC were comparable.
Conclusions
Despite significant differences in collateralization, the infarct patterns and severity of CVRC impairment do not differ between MMV and ACVD patients. Cerebral collateralization does not allow reaching conclusions about the localization of cerebral ischemia or severity of impaired CVRC in chronic hemodynamic impairment.




Similar content being viewed by others
References
Campbell BC, Christensen S, Tress BM, Churilov L, Desmond PM, Parsons MW, Barber PA, Levi CR, Bladin C, Donnan GA, Davis SM (2013) Failure of collateral blood flow is associated with infarct growth in ischemic stroke. J Cereb Blood Flow Metab 33:1168–1172
Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, Janis LS, Lutsep HL, Barnwell SL, Waters MF, Hoh BL, Hourihane JM, Levy EI, Alexandrov AV, Harrigan MR, Chiu D, Klucznik RP, Clark JM, McDougall CG, Johnson MD, Pride GL Jr, Torbey MT, Zaidat OO, Rumboldt Z, Cloft HJ (2011) Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 365:993–1003
Conklin J, Fierstra J, Crawley AP, Han JS, Poublanc J, Silver FL, Tymianski M, Fisher JA, Mandell DM, Mikulis DJ (2011) Mapping white matter diffusion and cerebrovascular reactivity in carotid occlusive disease. Neurology 77:431–438
Czabanka M, Pena-Tapia P, Scharf J, Schubert GA, Munch E, Horn P, Schmiedek P, Vajkoczy P (2011) Characterization of direct and indirect cerebral revascularization for the treatment of European patients with moyamoya disease. Cerebrovasc Dis 32:361–369
Czabanka M, Pena-Tapia P, Schubert GA, Woitzik J, Horn P, Schmiedek P, Vajkoczy P (2009) Clinical implications of cortical microvasculature in adult moyamoya disease. J Cereb Blood Flow Metab 29:1383–1387
Czabanka M, Pena-Tapia P, Schubert GA, Woitzik J, Vajkoczy P, Schmiedek P (2008) Characterization of cortical microvascularization in adult moyamoya disease. Stroke 39:1703–1709
Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS, Montgomery J, Nizam A, Lane BF, Lutsep HL, Barnwell SL, Waters MF, Hoh BL, Hourihane JM, Levy EI, Alexandrov AV, Harrigan MR, Chiu D, Klucznik RP, Clark JM, McDougall CG, Johnson MD, Pride GL, Jr., Lynch JR, Zaidat OO, Rumboldt Z, Cloft HJ (2013) Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet
Forster A, Szabo K, Hennerici MG (2008) Pathophysiological concepts of stroke in hemodynamic risk zones—do hypoperfusion and embolism interact? Nat Clin Pract Neurol 4:216–225
Fukui M (1997) Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis (‘moyamoya’ disease). Research committee on spontaneous occlusion of the circle of Willis (moyamoya disease) of the Ministry of Health and Welfare, Japan. Clin Neurol Neurosurg 99(Suppl 2):S238–S240
Grubb RL Jr, Powers WJ, Clarke WR, Videen TO, Adams HP Jr, Derdeyn CP (2013) Surgical results of the carotid occlusion surgery study. J Neurosurg 118:25–33
Hecht N, He J, Kremenetskaia I, Nieminen M, Vajkoczy P, Woitzik J (2012) Cerebral hemodynamic reserve and vascular remodeling in C57/BL6 mice are influenced by age. Stroke 43:3052–3062
Kraemer M, Heienbrok W, Berlit P (2008) Moyamoya disease in Europeans. Stroke 39:3193–3200
Liebeskind DS (2003) Collateral circulation. Stroke 34:2279–2284
Liebeskind DS (2012) Collateral perfusion: time for novel paradigms in cerebral ischemia. Int J Stroke 7:309–310
Liebeskind DS (2005) Location, location, location: angiography discerns early MR imaging vessel signs due to proximal arterial occlusion and distal collateral flow. AJNR Am J Neuroradiol 26:2432–2433, author reply 2433–4
Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Cloft HJ, Chimowitz MI (2011) Collateral circulation in symptomatic intracranial atherosclerosis. J Cereb Blood Flow Metab 31:1293–1301
Moossy J (1993) Pathology of cerebral atherosclerosis. Influence of age, race, and gender. Stroke 24(I22–3):I31–I32
Mugikura S, Takahashi S, Higano S, Shirane R, Kurihara N, Furuta S, Ezura M, Takahashi A (1999) The relationship between cerebral infarction and angiographic characteristics in childhood moyamoya disease. AJNR Am J Neuroradiol 20:336–343
Rafat N, Beck G, Pena-Tapia PG, Schmiedek P, Vajkoczy P (2009) Increased levels of circulating endothelial progenitor cells in patients with moyamoya disease. Stroke 40:432–438
Schmiedek P, Piepgras A, Leinsinger G, Kirsch CM, Einhupl K (1994) Improvement of cerebrovascular reserve capacity by EC-IC arterial bypass surgery in patients with ICA occlusion and hemodynamic cerebral ischemia. J Neurosurg 81:236–244
Schubert GA, Czabanka M, Seiz M, Horn P, Vajkoczy P, Thome C (2014) Perfusion characteristics of moyamoya disease: an anatomically and clinically oriented analysis and comparison. Stroke 45:101–106
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360:1226–1237
Shuaib A, Butcher K, Mohammad AA, Saqqur M, Liebeskind DS (2011) Collateral blood vessels in acute ischaemic stroke: a potential therapeutic target. Lancet Neurol 10:909–921
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Ture U, Yasargil MG, Krisht AF (1996) The arteries of the corpus callosum: a microsurgical anatomic study. Neurosurgery 39:1075–1084, discussion 1084–5
Vajkoczy P (2009) Moyamoya disease: collateralization is everything. Cerebrovasc Dis 28:258
Acknowledgments
The authors have nothing to acknowledge. This work was funded by the NeuroCure Flexible Fund 2010, Universitätsmedizin Charité, Berlin, and by the “Friedrich C. Luft” Clinical Scientist Pilot Program (funded by the Volkswagen Foundation and Charité Foundation).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
These authors tested a hypothesis (not directly stated) that collateral flow, ischemic reserve and infarct patterns would differ between moyamoya ischemia, with the potential for collateral recruitment, and atherosclerotic ischemic, where the potential might be less so. This was done in a population of surgical patients who received either direct or indirect bypass procedures. An extensive preoperative workup included evaluation of the functional reserve with either xenon-CT or SPECT, evaluation of arterial anastomoses with angiography and infarct evaluation with MRI diffusion/perfusion.
Anatomical flow patterns differed, with more ACoA anastomoses in the ASCVD patients and more PComA collateral flow in the moyamoya patients. Curiously, extracranial to intracranial anastomoses were frequently seen in both. Notwithstanding these differences, ischemic patterns appeared to be about the same in both frequency and anatomical distribution. Likewise, CV reserve capacities were similar between the two groups, despite the anatomical differences in collateral supply.
The “unstated” hypothesis is thus disproved. The work is elegant and fascinating from a physiologic standpoint. [Our own concept of experimental collateral circulation, somewhat different, was published some time ago (1).] But of course we would like to see more, most specifically, what were the results of all three evaluation modalities after bypass, can bypass type be specified or predicted by preoperative data, and what are the clinical outcomes post bypass? We look forward to further investigations by this obviously sophisticated group.
Christopher Miranda Loftus
Illinois, USA
1. Loftus CM, Greene GM, Detailer KN, Baumbach GL, Harrison DG, Heistad DD: Studies of collateral perfusion to canine middle cerebral artery territory. Am J Physiol. 259 (Heart Circ. Physiol.28):H560-H566, 1990.
Rights and permissions
About this article
Cite this article
Czabanka, M., Acker, G., Jussen, D. et al. Collateralization and ischemia in hemodynamic cerebrovascular insufficiency. Acta Neurochir 156, 2051–2058 (2014). https://doi.org/10.1007/s00701-014-2227-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2227-1