Abstract
Purpose
The objective of our study was to evaluate the safety and accuracy of ultrasound (US) compared to standard radiographs in diagnosing supracondylar fractures (SCFs) of the humerus in children.
Patients and methods
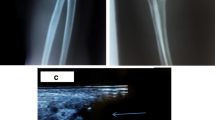
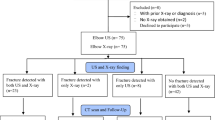
A total of 106 children (aged between 1 and 13 years) with clinically suspected SCF of the humerus were primarily examined by US followed by standard two-plane radiographs of the elbow. US was conducted with a linear scanner viewing the distal humerus from seven standardized sectional planes. US fracture diagnosis was established either by a cortical bulging or cortical gap, or by a positive dorsal fat pad (dFP) sign. X-ray diagnosis was stated by an independent pediatric radiologist and, afterwards, compared to our US findings. Sonographic and radiographic findings were collected in a contingency table. The sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) for US fracture diagnosis were calculated according to the radiographs. In addition, by identifying significant angulation and/or disrupture, SCFs were classified as non-operative/stable and operative/instable SCFs according to the AO Pediatric Fracture Classification System.
Results
By US, a SCF could be excluded in 43 patients and in 63 patients, a fracture was diagnosed. In contrast, by radiographs, an SCF could be excluded in 46 patients and in 60 patients, a fracture was diagnosed. For US fracture diagnosis in comparison to radiographs, we calculated a sensitivity of 100 %, a specificity of 93.5 %, an NPV of 100 %, and a PPV of 95.2 %. Thirty-nine SCFs were sonographically classified as stable grades 1/2 SCFs and confirmed in 37 patients by X-rays. All four operative/instable SCFs were correctly identified by US.
Conclusion
By identifying a positive dFP sign and/or cortical lesions of the distal humerus, SCFs can be detected very sensitively by US. Even the estimation of fracture displacement seems to be possible. We suggest US as an applicable alternative method in the primary evaluation of suspected SCF in children, guiding further diagnostics, where appropriate. After minor injuries, if clinical assessment for an elbow fracture is low and US examination is negative for fracture, additional radiographs are dispensable. Thereby, the amount of X-ray burden during childhood can be reduced, without loss of diagnostic safety.








Similar content being viewed by others
References
Minkowitz B, Busch MT. Supracondylar humerus fractures. Current trends and controversies. Orthop Clin North Am. 1994;25(4):581–94.
Hell A, Weinberg A-M, Kraus R, Haxhija E. Kapitel 14 Ellbogen. In: Weinberg A-M, Tscherne H, Henkel R, editors. Unfallchirurgie im Kindesalter. Berlin Heidelberg: Springer; 2006. p. 253–95.
Bache E. Elbow injuries. In: Baert AL, Johnson KJ, Bache E, editors. Imaging in pediatric skeletal trauma: techniques and applications. 1st ed. Berlin Heidelberg New York: Springer; 2008. p. 257–80.
Alzen G, Duque-Reina D, Urhahn R, et al. Radiographic examination of injuries in children. Clinical and legal considerations about indications. Dtsch Med Wochenschr. 1992;117:363–7.
Alzen G, Benz-Bohm G. Radiation protection in pediatric radiology. Dtsch Arztebl Int. 2011;108(24):407–14.
Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A. 2003;100(24):13761–6.
Brix G, Nekolla E, Griebel J. Radiation exposure of patients from diagnostic and interventional X-ray procedures. Facts, assessment and trends. Radiologe. 2005;45:340–9.
Fletcher EW, Baum JD, Draper G. The risk of diagnostic radiation of the newborn. Br J Radiol. 1986;59(698):165–70.
Linet MS, Kim K, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol. 2009;39(Suppl 1):S4–26.
Rathfelder FJ, Paar O. Ultrasound as an alternative diagnostic measure for fractures during the growth phase. Unfallchirurg. 1995;98:645–9.
Moritz JD, Berthold LD, Soenksen SF, et al. Ultrasound in diagnosis of fractures in children: unnecessary harassment or useful addition to X-ray? Ultraschall Med. 2008;29(3):267–74.
Moritz JD, Hoffmann B, Meuser SH, et al. Is ultrasound equal to X-ray in pediatric fracture diagnosis? Rofo. 2010;182:706–14.
Hübner U, Schlicht W, Outzen S, et al. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg Br. 2000;82(8):1170–3.
Ackermann O, Liedgens P, Eckert K, et al. Sonographische Diagnostik von metaphysären Wulstbrüchen. Unfallchirurg. 2009;112:706–11.
Ackermann O, Sesia S, Berberich T, et al. Sonographische Diagnostik der subcapitalen Humerusfraktur im Wachstumsalter. Unfallchirurg. 2010;113:839–44.
Chaar-Alvarez FM, Warkentine F, Cross K, et al. Bedside ultrasound diagnosis of nonangulated distal forearm fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27:1027–32.
Eckert K, Ackermann O, Schweiger B, et al. Ultrasound as a viable alternative to standard X-rays for the diagnosis of distal forearm fractures in children. Z Orthop Unfall. 2012;150(4):409–14.
Eckert K, Ackermann O, Schweiger B, et al. Sonographic diagnosis of metaphyseal forearm fractures in children: a safe and applicable alternative to standard X-rays. Pediatr Emerg Care. 2012;28(9):851–4.
Pountos I, Clegg J, Siddiqui A. Diagnosis and treatment of greenstick and torus fractures of the distal radius in children: a prospective randomised single blind study. J Child Orthop. 2010;4:321–6.
Williamson D, Watura R, Cobby M. Ultrasound imaging of forearm fractures in children: a viable alternative? J Accid Emerg Med. 2000;17:22–4.
Ackermann O, Sesia S, Berberich T, et al. Evaluation of proximal humerus fractures in children with ultrasonography a prospective multicenter study. Eur J Trauma Emerg Surg. 2011;37:322.
Chien M, Bulloch B, Garcia-Filion P, et al. Bedside ultrasound in the diagnosis of pediatric clavicle fractures. Pediatr Emerg Care. 2011;27:1038–41.
Barr LL, Babcock DS. Sonography of the normal elbow. AJR Am J Roentgenol. 1991;157(4):793–8.
Finlay K, Ferri M, Friedman L. Ultrasound of the elbow. Skeletal Radiol. 2004;33:63–79.
Grechenig W, Clement H, Schatz B, et al. Ultrasonographic diagnosis of fractures—an experimental study. Biomed Technik. 1997;42:138–45.
Grechenig W, Mayr J, Fellinger M, et al. Sonographic anatomy and pathologic findings of the elbow joint in children and adults. Radiologe. 1998;38:378–89.
Grechenig W, Clement HG, Schatz B, et al. Sonographic examination of trauma to the elbow and hand. Orthopäde. 2002;31:271–7.
Konermann W, Gruber G. Standard ultrasound sections of the upper extremity—shoulder and elbow joint. Ultraschall Med. 1998;19:130–8.
Konermann W, Gruber G. Allgemeiner Teil. In: Konermann W, Gruber G, editors. Ultraschalldiagnostik der Stütz- und Bewegungsorgane. Stuttgart: Thieme; 2000. p. 1–38.
Markowitz RI, Davidson RS, Harty MP, et al. Sonography of the elbow in infants and children. AJR Am J Roentgenol. 1992;159:829–33.
Martinoli C, Bianchi S, Zamorani MP, et al. Ultrasound of the elbow. Eur J Ultrasound. 2001;14:21–7.
Martinoli C, Bianchi S, Giovagnorio F, et al. Ultrasound of the elbow. Skeletal Radiol. 2001;30:605–14.
Tran N, Chow K. Ultrasonography of the elbow. Semin Musculoskelet Radiol. 2007;11:105–16.
Davidson RS, Markowitz RI, Dormans J, et al. Ultrasonographic evaluation of the elbow in infants and young children after suspected trauma. J Bone Joint Surg Am. 1994;76(12):1804–13.
Pistor G, Graffstädt H. Sonographic diagnosis of supracondylar fractures of the humerus—retrospective and prospective studies in children. Ultraschall Med. 2003;24:331–9.
Vocke-Hell AK, Schmid A. Sonographic differentiation of stable and unstable lateral condyle fractures of the humerus in children. J Pediatr Orthop B. 2001;10(2):138–41.
Zhang JD, Chen H. Ultrasonography for non-displaced and mini-displaced humeral lateral condyle fractures in children. Chin J Traumatol. 2008;11(5):297–300.
Ziv N, Litwin A, Katz K, et al. Definitive diagnosis of fracture-separation of the distal humeral epiphysis in neonates by ultrasonography. Pediatr Radiol. 1996;26(7):493–6.
Zuazo I, Bonnefoy O, Tauzin C, et al. Acute elbow trauma in children: role of ultrasonography. Pediatr Radiol. 2008;38:982–8.
Slongo T, Audigé L, Schlickewei W, et al. Development and validation of the AO pediatric comprehensive classification of long bone fractures by the Pediatric Expert Group of the AO foundation in collaboration with AO Clinical Investigation and Documentation and the International Association for Pediatric Traumatology. J Pediatr Orthop. 2006;26(1):43–9.
Lutz N, Audigé L, Schmittenbecher P, et al. Diagnostic algorithm for a validated displacement grading of pediatric supracondylar fractures. J Pediatr Orthop. 2011;31(2):117–23.
Rabiner JE, Khine H, Avner JR, et al. Accuracy of point-of-care ultrasonography for diagnosis of elbow fractures in children. Ann Emerg Med. 2013;61(1):9–17.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eckert, K., Janssen, N., Ackermann, O. et al. Ultrasound diagnosis of supracondylar fractures in children. Eur J Trauma Emerg Surg 40, 159–168 (2014). https://doi.org/10.1007/s00068-013-0306-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-013-0306-2