Abstract
To meet the growing need for tissue replacement materials for our aging population, the development of new adaptive biomaterials is essential. The tissues with the highest demand for implant materials are skin and bone. These tissues share various similarities, including signaling pathways and extracellular matrix composition. Glycosaminoglycans such as hyaluronan and chondroitin sulfate are the major organic extracellular matrix components. They modulate the attraction of skin and bone precursor cells and their subsequent differentiation and gene expression and regulate the action of proteins essential to bone and skin regeneration. The precise action of glycosaminoglycans varies according to their structural composition mainly in respect to the degree of sulfation and polymer length. Changes in the glycosaminoglycan composition are frequently seen in physiological and pathological remodeling processes, such as bone formation or scaring. Here, we review the current state of knowledge of how the most common glycosaminoglycan, chondroitin sulfate and hyaluronan, interact with bone and skin cells, and summarize their potential in tissue engineering for skeletal and skin diseases.



Similar content being viewed by others
References
Mathieu LM, Mueller TL, Bourban PE, Pioletti DP, Muller R, Manson JA (2006) Architecture and properties of anisotropic polymer composite scaffolds for bone tissue engineering. Biomaterials 27:905–916
Fini M, Giavaresi G, Torricelli P, Borsari V, Giardino R, Nicolini A, Carpi A (2004) Osteoporosis and biomaterial osteointegration. Biomed Pharmacother 58:487–493
Scharnweber D, Beutner R, Roessler S, Michael J, Schwenzer B (2009) Using electrochemical approaches for bio surface engineering of titanium based implants. In Karlinsey RL (ed) Recent developments in advanced medical and dental materials using electrochemical methodologies. Research Signpost
Bierbaum S, Scharnweber D (2010) Artificial extracellular matrices to functionalize biomaterial surfaces. Elsevier, Amsterdam
Freyman TM, Yannas IV, Gibson LJ (2001) Cellular materials as porous scaffolds for tissue engineering. Progr Mater Sci 46:273–282
Ross FP, Christiano AM (2006) Nothing but skin and bone. J Clin Invest 116:1140–1149
Jahoda CA, Whitehouse J, Reynolds AJ, Hole N (2003) Hair follicle dermal cells differentiate into adipogenic and osteogenic lineages. Exp Dermatol 12:849–859
Lako M, Armstrong L, Cairns PM, Harris S, Hole N, Jahoda CA (2002) Hair follicle dermal cells repopulate the mouse haematopoietic system. J Cell Sci 115:3967–3974
Loser K, Mehling A, Loeser S, Apelt J, Kuhn A, Grabbe S, Schwarz T, Penninger JM, Beissert S (2006) Epidermal RANKL controls regulatory T-cell numbers via activation of dendritic cells. Nat Med 12:1372–1379
Khosla S, Westendorf JJ, Oursler MJ (2008) Building bone to reverse osteoporosis and repair fractures. J Clin Invest 118:421–428
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Ruggiero F, Roulet M, Bonod-Bidaud C (2005) Dermis collagens: beyond their structural properties. J Soc Biol 199:301–311
Robey PG, Boskey AL (2009) The composition of bone. In: ASBMR (ed.) Primer on the metabolic bone diseases and disorders of mineral metabolism. Wiley, Hoboken
Wagner DO, Aspenberg P (2011) Where did bone come from? Acta Orthop 82:1–6. doi:10.3109/17453674.2011.588861
Gandhi NS, Mancera RL (2008) The structure of glycosaminoglycans and their interactions with proteins. Chem Biol Drug Des 72:455–482. doi:10.1111/j.1747-0285.2008.00741.x
Esko JD, Kimata K, Lindahl U (2009) Proteoglycans and sulfated glycosaminoglycans. In: Varki A et al (eds) Essentials of glycobiology, 2nd edn. Cold Spring Harbor Laboratory Press, Cold Spring Harbor
Pieper JS, van Wachem PB, van Luyn MJA, Brouwer LA, Hafmans T, Veerkamp JH, van Kuppevelt TH (2000) Attachment of glycosaminoglycans to collagenous matrices modulates the tissue response in rats. Biomaterials 21:1689–1699
Roughley PJ (2006) The structure and function of cartilage proteoglycans. Eur Cell Mater 12:92–101
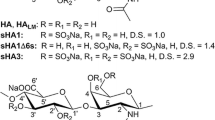
Hintze V, Moeller S, Schnabelrauch M, Bierbaum S, Viola M, Worch H, Scharnweber D (2009) Modifications of hyaluronan influence the interaction with human bone morphogenetic protein-4 (hBMP-4). Biomacromolecules 10:3290–3297
Sasisekharan R, Raman R, Prabhakar V (2006) Glycomics approach to structure-function relationships of glycosaminoglycans. Annu Rev Biomed Eng 8:181–231
Souza-Fernandes AB, Pelosi P, Rocco PR (2006) Bench-to-bedside review: the role of glycosaminoglycans in respiratory disease. Crit Care 10:237
Kunze R, Rosler M, Moller S, Schnabelrauch M, Riemer T, Hempel U, Dieter P (2009) Sulfated hyaluronan derivatives reduce the proliferation rate of primary rat calvarial osteoblasts. Glycoconj J 27:151–158
Lamoureux F, Baud’huin M, Duplomb L, Heymann D, Redini F (2007) Proteoglycans: key partners in bone cell biology. Bioessays 29:758–771. doi:10.1002/bies.20612
Prestwich GD (2008) Engineering a clinically-useful matrix for cell therapy. Organogenesis 4:42–47
Ling L, Murali S, Stein GS, van Wijnen AJ, Cool SM (2010) Glycosaminoglycans modulate RANKL-induced osteoclastogenesis. J Cell Biochem 109:1222–1231
Docherty R, Forrester JV, Lackie JM, Gregory DW (1989) Glycosaminoglycans facilitate the movement of fibroblasts through three-dimensional collagen matrices. J Cell Sci 92(Pt 2):263–270
Zhang L (2010) Glycosaminoglycan (GAG) biosynthesis and GAG-binding proteins. Prog Mol Biol Transl Sci 93:1–17
Grzesik WJ, Frazier CR, Shapiro JR, Sponseller PD, Robey PG, Fedarko NS (2002) Age-related changes in human bone proteoglycan structure. Impact of osteogenesis imperfecta. J Biol Chem 277:43638–43647
Bernstein EF, Underhill CB, Hahn PJ, Brown DB, Uitto J (1996) Chronic sun exposure alters both the content and distribution of dermal glycosaminoglycans. Br J Dermatol 135:255–262
Willen MD, Sorrell JM, Lekan CC, Davis BR, Caplan AI (1991) Patterns of glycosaminoglycan/proteoglycan immunostaining in human skin during aging. J Invest Dermatol 96:968–974
Hubbell JA (2003) Materials as morphogenetic guides in tissue engineering. Curr Opin Biotechnol 14:551–558
Pieper JS, Oosterhof A, Dijkstra PJ, Veerkamp JH, van Kuppevelt TH (1999) Preparation and characterization of porous crosslinked collagenous matrices containing bioavailable chondroitin sulphate. Biomaterials 20:847–858
Tierney CM, Jaasma MJ, O'Brien FJ (2009) Osteoblast activity on collagen-GAG scaffolds is affected by collagen and GAG concentrations. J Biomed Mater Res A 91:92–101
Mania VM, Kallivokas AG, Malavaki C, Asimakopoulou AP, Kanakis J, Theocharis AD, Klironomos G, Gatzounis G, Mouzaki A, Panagiotopoulos E et al (2009) A comparative biochemical analysis of glycosaminoglycans and proteoglycans in human orthotopic and heterotopic bone. IUBMB Life 61:447–452. doi:10.1002/iub.167
Maccari F, Volpi N (2008) Structural characterization of the skin glycosaminoglycans in patients with pseudoxanthoma elasticum. Int J Dermatol 47:1024–1027. doi:10.1111/j.1365-4632.2008.03762.x
Waddington RJ, Langley MS (1998) Structural analysis of proteoglycans synthesized by mineralizing bone cells in vitro in the presence of fluoride. Matrix Biol 17:255–268
Catini C, Gheri G (1990) The GAGs of the bone: a study on human calva. Arch Ital Anat Embriol 95:237–240
Waddington RJ, Embery G, Last KS (1989) Glycosaminoglycans of human alveolar bone. Arch Oral Biol 34:587–589
Vejlens L (1971) Glycosaminoglycans of human bone tissue. I. Pattern of compact bone in relation to age. Calcif Tissue Res 7:175–190
Prince CW, Navia JM (1983) Glycosaminoglycan alterations in rat bone due to growth and fluorosis. J Nutr 113:1576–1582
Olczyk P, Komosinska-Vassev K, Winsz-Szczotka K, Kuznik-Trocha K, Olczyk K (2008) Hyaluronan: structure, metabolism, functions, and role in wound healing. Postepy Hig Med Dosw (Online) 62:651–659
Hascall V, Esko JD (2009) Hyaluronan. In: Varki A et al (eds) Essentials of glycobiology, 2nd edn. Cold Spring Harbor Laboratory Press, Cold Spring Harbor
Lokeshwar VB, Selzer MG (2000) Differences in hyaluronic acid-mediated functions and signaling in arterial, microvessel, and vein-derived human endothelial cells. J Biol Chem 275:27641–27649
Ponta H, Sherman L, Herrlich PA (2003) CD44: from adhesion molecules to signalling regulators. Nat Rev Mol Cell Biol 4:33–45
Pivetta E, Scapolan M, Wassermann B, Steffan A, Colombatti A, Spessotto P (2011) Blood-derived human osteoclast resorption activity is impaired by hyaluronan-CD44 engagement via a p38-dependent mechanism. J Cell Physiol 226:769–779
Ruffell B, Poon GF, Lee SS, Brown KL, Tjew SL, Cooper J, Johnson P (2011) Differential use of chondroitin sulfate to regulate hyaluronan binding by receptor CD44 in inflammatory and interleukin 4-activated macrophages. J Biol Chem 286:19179–19190
Bastow ER, Byers S, Golub SB, Clarkin CE, Pitsillides AA, Fosang AJ (2008) Hyaluronan synthesis and degradation in cartilage and bone. Cell Mol Life Sci 65:395–413
Sterling H, Saginario C, Vignery A (1998) CD44 occupancy prevents macrophage multinucleation. J Cell Biol 143:837–847
Cui W, Ke JZ, Zhang Q, Ke HZ, Chalouni C, Vignery A (2006) The intracellular domain of CD44 promotes the fusion of macrophages. Blood 107:796–805
Turley EA (1982) Purification of a hyaluronate-binding protein fraction that modifies cell social behavior. Biochem Biophys Res Commun 108:1016–1024
Turley EA, Austen L, Vandeligt K, Clary C (1991) Hyaluronan and a cell-associated hyaluronan binding protein regulate the locomotion of ras-transformed cells. J Cell Biol 112:1041–1047
Silbert JE, Sugumaran G (2002) Biosynthesis of chondroitin/dermatan sulfate. IUBMB Life 54:177–186
Lamari FN, Karamanos NK (2006) Structure of chondroitin sulfate. Academic, New York
Saito A, Munakata H (2004) Detection of chondroitin sulfate-binding proteins on the membrane. Electrophoresis 25:2452–2460
Kirschfink M, Blase L, Engelmann S, Schwartz-Albiez R (1997) Secreted chondroitin sulfate proteoglycan of human B cell lines binds to the complement protein C1q and inhibits complex formation of C1. J Immunol 158:1324–1331
Miyazaki T, Miyauchi S, Tawada A, Anada T, Suzuki O (2010) Effect of chondroitin sulfate-E on the osteoclastic differentiation of RAW264 cells. Dent Mater J 29:403–410
Gama, Cristal I, Tully, Sarah E, Hsieh-wilson, Linda C (2007) Chondroitin sulfate binding proteins and modulators thereof United States California Institute of Technology. http://www.freepatentsonline.com/y2007/0275412.html
Zhu W, Robey PG, Boskey AL (2008) Osteoporosis, 3rd edn. Elsevier, San Diego
Hadjidakis DJ, Androulakis II (2006) Bone remodeling. Ann N Y Acad Sci 1092:385–396
van der Harst MR, Brama PA, van de Lest CH, Kiers GH, DeGroot J, van Weeren PR (2004) An integral biochemical analysis of the main constituents of articular cartilage, subchondral and trabecular bone. Osteoarthritis Cartilage 12:752–761
Haupt LM, Murali S, Mun FK, Teplyuk N, Mei LF, Stein GS, van Wijnen AJ, Nurcombe V, Cool SM (2009) The heparan sulfate proteoglycan (HSPG) glypican-3 mediates commitment of MC3T3-E1 cells toward osteogenesis. J Cell Physiol 220:780–791
Hoshiba T, Kawazoe N, Tateishi T, Chen G (2009) Development of stepwise osteogenesis-mimicking matrices for the regulation of mesenchymal stem cell functions. J Biol Chem 284:31164–31173
Irie A, Takami M, Kubo H, Sekino-Suzuki N, Kasahara K, Sanai Y (2007) Heparin enhances osteoclastic bone resorption by inhibiting osteoprotegerin activity. Bone 41:165–174
Ariyoshi W, Takahashi T, Kanno T, Ichimiya H, Takano H, Koseki T, Nishihara T (2005) Mechanisms involved in enhancement of osteoclast formation and function by low molecular weight hyaluronic acid. J Biol Chem 280:18967–18972
Ariyoshi W, Takahashi T, Kanno T, Ichimiya H, Shinmyouzu K, Takano H, Koseki T, Nishihara T (2008) Heparin inhibits osteoclastic differentiation and function. J Cell Biochem 103:1707–1717
Lion JM, Mentaverri R, Rossard S, Jullian N, Courtois B, Courtois J, Brazier M, Maziere JC, Kamel S (2009) Oligogalacturonic acid inhibit bone resorption and collagen degradation through its interaction with type I collagen. Biochem Pharmacol 78:1448–1455
Li Z, Hou WS, Escalante-Torres CR, Gelb BD, Bromme D (2002) Collagenase activity of cathepsin K depends on complex formation with chondroitin sulfate. J Biol Chem 277:28669–28676
Prince CW (2004) Roles of hyaluronan in bone resorption. BMC Musculoskelet Disord 5:12
Zimmerman E, Geiger B, Addadi L (2002) Initial stages of cell-matrix adhesion can be mediated and modulated by cell-surface hyaluronan. Biophys J 82:1848–1857
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423:337–342
Del Fattore A, Teti A, Rucci N (2008) Osteoclast receptors and signaling. Arch Biochem Biophys 473:147–160
Khosla S (2001) Minireview: the OPG/RANKL/RANK system. Endocrinology 142:5050–5055
Trouvin AP, Goeb V (2010) Receptor activator of nuclear factor-kappaB ligand and osteoprotegerin: maintaining the balance to prevent bone loss. Clin Interv Aging 5:345–354
Schoppet M, Preissner KT, Hofbauer LC (2002) RANK ligand and osteoprotegerin: paracrine regulators of bone metabolism and vascular function. Arterioscler Thromb Vasc Biol 22:549–553
Theoleyre S, Kwan Tat S, Vusio P, Blanchard F, Gallagher J, Ricard-Blum S, Fortun Y, Padrines M, Redini F, Heymann D (2006) Characterization of osteoprotegerin binding to glycosaminoglycans by surface plasmon resonance: role in the interactions with receptor activator of nuclear factor kappaB ligand (RANKL) and RANK. Biochem Biophys Res Commun 347:460–467
Lamoureux F, Picarda G, Garrigue-Antar L, Baud’huin M, Trichet V, Vidal A, Miot-Noirault E, Pitard B, Heymann D, Redini F (2009) Glycosaminoglycans as potential regulators of osteoprotegerin therapeutic activity in osteosarcoma. Cancer Res 69:526–536
Velasco CR, Colliec-Jouault S, Redini F, Heymann D, Padrines M (2010) Proteoglycans on bone tumor development. Drug Discov Today 15:553–560
Chang EJ, Kim HJ, Ha J, Kim HJ, Ryu J, Park KH, Kim UH, Lee ZH, Kim HM, Fisher DE et al (2007) Hyaluronan inhibits osteoclast differentiation via Toll-like receptor 4. J Cell Sci 120:166–176
Luben RA, Goggins JF, Raisz LG (1974) Stimulation by parathyroid hormone of bone hyaluronate synthesis in organ culture. Endocrinology 94:737–745
Baud’huin M, Ruiz-Velasco C, Jego G, Charrier C, Gasiunas N, Gallagher J, Maillasson M, Naggi A, Padrines M, Redini F et al (2010) Glycosaminoglycans inhibit the adherence and the spreading of osteoclasts and their precursors: role in osteoclastogenesis and bone resorption. Eur J Cell Biol 90:49–57
Chabadel A, Banon-Rodriguez I, Cluet D, Rudkin BB, Wehrle-Haller B, Genot E, Jurdic P, Anton IM, Saltel F (2007) CD44 and beta3 integrin organize two functionally distinct actin-based domains in osteoclasts. Mol Biol Cell 18:4899–4910
Saltel F, Chabadel A, Bonnelye E, Jurdic P (2008) Actin cytoskeletal organisation in osteoclasts: a model to decipher transmigration and matrix degradation. Eur J Cell Biol 87:459–468
Alliston T (2010) Chondroitin sulfate and growth factor signaling in the skeleton: possible links to MPS VI. J Pediatr Rehabil Med 3:129–138
Ruffell B, Johnson P (2005) Chondroitin sulfate addition to CD44H negatively regulates hyaluronan binding. Biochem Biophys Res Commun 334:306–312
Schneiders W, Reinstorf A, Biewener A, Serra A, Grass R, Kinscher M, Heineck J, Rehberg S, Zwipp H, Rammelt S (2009) In vivo effects of modification of hydroxyapatite/collagen composites with and without chondroitin sulphate on bone remodeling in the sheep tibia. J Orthop Res 27:15–21
Schneiders W, Reinstorf A, Ruhnow M, Rehberg S, Heineck J, Hinterseher I, Biewener A, Zwipp H, Rammelt S (2008) Effect of chondroitin sulphate on material properties and bone remodelling around hydroxyapatite/collagen composites. J Biomed Mater Res A 85:638–645
Rammelt S, Heck C, Bernhardt R, Bierbaum S, Scharnweber D, Goebbels J, Ziegler J, Biewener A, Zwipp H (2007) In vivo effects of coating loaded and unloaded Ti implants with collagen, chondroitin sulfate, and hydroxyapatite in the sheep tibia. J Orthop Res 25:1052–1061
Simonaro CM, D’Angelo M, He X, Eliyahu E, Shtraizent N, Haskins ME, Schuchman EH (2008) Mechanism of glycosaminoglycan-mediated bone and joint disease: implications for the mucopolysaccharidoses and other connective tissue diseases. Am J Pathol 172:112–122
Pittenger MF (2008) Mesenchymal stem cells from adult bone marrow. Methods Mol Biol 449:27–44
Lynch MP, Capparelli C, Stein JL, Stein GS, Lian JB (1998) Apoptosis during bone-like tissue development in vitro. J Cell Biochem 68:31–49
Lian JB, Javed A, Zaidi SK, Lengner C, Montecino M, van Wijnen AJ, Stein JL, Stein GS (2004) Regulatory controls for osteoblast growth and differentiation: role of Runx/Cbfa/AML factors. Crit Rev Eukaryot Gene Expr 14:1–41
Becker D, Geissler U, Hempel U, Bierbaum S, Scharnweber D, Worch H, Wenzel KW (2002) Proliferation and differentiation of rat calvarial osteoblasts on type I collagen-coated titanium alloy. J Biomed Mater Res 59:516–527
Augello A, Kurth TB, De Bari C (2010) Mesenchymal stem cells: a perspective from in vitro cultures to in vivo migration and niches. Eur Cell Mater 20:121–133
Chen XD (2010) Extracellular matrix provides an optimal niche for the maintenance and propagation of mesenchymal stem cells. Birth Defects Res C Embryo Today 90:45–54
Jackson RA, Murali S, van Wijnen AJ, Stein GS, Nurcombe V, Cool SM (2007) Heparan sulfate regulates the anabolic activity of MC3T3-E1 preosteoblast cells by induction of Runx2. J Cell Physiol 210:38–50
Dombrowski C, Song SJ, Chuan P, Lim X, Susanto E, Sawyer AA, Woodruff MA, Hutmacher DW, Nurcombe V, Cool SM (2009) Heparan sulfate mediates the proliferation and differentiation of rat mesenchymal stem cells. Stem Cells Dev 18:661–670
Nikitovic D, Zafiropoulos A, Tzanakakis GN, Karamanos NK, Tsatsakis AM (2005) Effects of glycosaminoglycans on cell proliferation of normal osteoblasts and human osteosarcoma cells depend on their type and fine chemical compositions. Anticancer Res 25:2851–2856
Miyazaki T, Miyauchi S, Tawada A, Anada T, Matsuzaka S, Suzuki O (2008) Oversulfated chondroitin sulfate-E binds to BMP-4 and enhances osteoblast differentiation. J Cell Physiol 217:769–777
Chen CC, Boskey AL (1985) Mechanisms of proteoglycan inhibition of hydroxyapatite growth. Calcif Tissue Int 37:395–400
Nagahata M, Tsuchiya T, Ishiguro T, Matsuda N, Nakatsuchi Y, Teramoto A, Hachimori A, Abe K (2004) A novel function of N-cadherin and Connexin43: marked enhancement of alkaline phosphatase activity in rat calvarial osteoblast exposed to sulfated hyaluronan. Biochem Biophys Res Commun 315:603–611
Baldwin AD, Kiick KL (2010) Polysaccharide-modified synthetic polymeric biomaterials. Biopolymers 94:128–140
Van Vlierberghe S, Dubruel P, Schacht E (2011) Biopolymer-based hydrogels as scaffolds for tissue engineering applications: a review. Biomacromolecules 12:1387–1408
Klim JR, Li L, Wrighton PJ, Piekarczyk MS, Kiessling LL (2010) A defined glycosaminoglycan-binding substratum for human pluripotent stem cells. Nat Methods 7:989–994
Luong-Van E, Grondahl L, Song S, Nurcombe V, Cool S (2007) The in vivo assessment of a novel scaffold containing heparan sulfate for tissue engineering with human mesenchymal stem cells. J Mol Histol 38:459–468
Farrell E, O’Brien FJ, Doyle P, Fischer J, Yannas I, Harley BA, O'Connell B, Prendergast PJ, Campbell VA (2006) A collagen-glycosaminoglycan scaffold supports adult rat mesenchymal stem cell differentiation along osteogenic and chondrogenic routes. Tissue Eng 12:459–468
Nagahata M, Nakaoka R, Teramoto A, Abe K, Tsuchiya T (2005) The response of normal human osteoblasts to anionic polysaccharide polyelectrolyte complexes. Biomaterials 26:5138–5144
Douglas T, Heinemann S, Mietrach C, Hempel U, Bierbaum S, Scharnweber D, Worch H (2007) Interactions of collagen types I and II with chondroitin sulfates A-C and their effect on osteoblast adhesion. Biomacromolecules 8:1085–1092
Douglas T, Hempel U, Mietrach C, Heinemann S, Scharnweber D, Worch H (2007) Fibrils of different collagen types containing immobilised proteoglycans (PGs) as coatings: characterisation and influence on osteoblast behaviour. Biomol Eng 24:455–458
Douglas T, Hempel U, Mietrach C, Viola M, Vigetti D, Heinemann S, Bierbaum S, Scharnweber D, Worch H (2008) Influence of collagen-fibril-based coatings containing decorin and biglycan on osteoblast behavior. J Biomed Mater Res A 84:805–816
Douglas T, Heinemann S, Hempel U, Mietrach C, Knieb C, Bierbaum S, Scharnweber D, Worch H (2008) Characterization of collagen II fibrils containing biglycan and their effect as a coating on osteoblast adhesion and proliferation. J Mater Sci Mater Med 19:1653–1660
Bierbaum S, Douglas T, Hanke T, Scharnweber D, Tippelt S, Monsees TK, Funk RH, Worch H (2006) Collageneous matrix coatings on titanium implants modified with decorin and chondroitin sulfate: characterization and influence on osteoblastic cells. J Biomed Mater Res A 77:551–562
Stadlinger B, Pilling E, Huhle M, Mai R, Bierbaum S, Scharnweber D, Kuhlisch E, Loukota R, Eckelt U (2008) Evaluation of osseointegration of dental implants coated with collagen, chondroitin sulphate and BMP-4: an animal study. Int J Oral Maxillofac Surg 37:54–59
Rider CC (2006) Heparin/heparan sulphate binding in the TGF-beta cytokine superfamily. Biochem Soc Trans 34:458–460
Shinmyouzu K, Takahashi T, Ariyoshi W, Ichimiya H, Kanzaki S, Nishihara T (2007) Dermatan sulfate inhibits osteoclast formation by binding to receptor activator of NF-kappa B ligand. Biochem Biophys Res Commun 354:447–452
Tammi R, Ripellino JA, Margolis RU, Tammi M (1988) Localization of epidermal hyaluronic acid using the hyaluronate binding region of cartilage proteoglycan as a specific probe. J Invest Dermatol 90:412–414
Gu H, Huang L, Wong YP, Burd A (2010) HA modulation of epidermal morphogenesis in an organotypic keratinocyte-fibroblast co-culture model. Exp Dermatol 19:e336–e339
Akimoto S, Hayashi H, Ishikawa H (1992) Disaccharide analysis of the skin glycosaminoglycans in systemic sclerosis. Br J Dermatol 126:29–34
Averbeck M, Gebhardt CA, Voigt S, Beilharz S, Anderegg U, Termeer CC, Sleeman JP, Simon JC (2007) Differential regulation of hyaluronan metabolism in the epidermal and dermal compartments of human skin by UVB irradiation. J Invest Dermatol 127:687–697
Gebhardt C, Averbeck M, Diedenhofen N, Willenberg A, Anderegg U, Sleeman JP, Simon JC (2010) Dermal hyaluronan is rapidly reduced by topical treatment with glucocorticoids. J Invest Dermatol 130:141–149
Ellis I, Banyard J, Schor SL (1997) Differential response of fetal and adult fibroblasts to cytokines: cell migration and hyaluronan synthesis. Development 124:1593–1600
Ellis IR, Schor AM, Schor SL (2007) EGF AND TGF-alpha motogenic activities are mediated by the EGF receptor via distinct matrix-dependent mechanisms. Exp Cell Res 313:732–741
Meran S, Luo DD, Simpson R, Martin J, Wells A, Steadman R, Phillips AO (2010) Hyaluronan facilitates transforming growth factor-beta1-dependent proliferation via CD44 and epidermal growth factor receptor interaction. J Biol Chem 286:17618–17630
Kobayashi H, Terao T (1997) Hyaluronic acid-specific regulation of cytokines by human uterine fibroblasts. Am J Physiol 273:C1151–C1159
Mutsaers SE, Bishop JE, McGrouther G, Laurent GJ (1997) Mechanisms of tissue repair: from wound healing to fibrosis. Int J Biochem Cell Biol 29:5–17
Sorokin L (2010) The impact of the extracellular matrix on inflammation. Nat Rev Immunol 10:712–723
Witt DP, Lander AD (1994) Differential binding of chemokines to glycosaminoglycan subpopulations. Curr Biol 4:394–400
Lawrence DA (1996) Transforming growth factor-beta: a general review. Eur Cytokine Netw 7:363–374
Yamawaki H, Hirohata S, Miyoshi T, Takahashi K, Ogawa H, Shinohata R, Demircan K, Kusachi S, Yamamoto K, Ninomiya Y (2009) Hyaluronan receptors involved in cytokine induction in monocytes. Glycobiology 19:83–92
Termeer C, Benedix F, Sleeman J, Fieber C, Voith U, Ahrens T, Miyake K, Freudenberg M, Galanos C, Simon JC (2002) Oligosaccharides of hyaluronan activate dendritic cells via toll-like receptor 4. J Exp Med 195:99–111
Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, Prestwich GD, Mascarenhas MM, Garg HG, Quinn DA et al (2005) Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nat Med 11:1173–1179
Gariboldi S, Palazzo M, Zanobbio L, Selleri S, Sommariva M, Sfondrini L, Cavicchini S, Balsari A, Rumio C (2008) Low molecular weight hyaluronic acid increases the self-defense of skin epithelium by induction of beta-defensin 2 via TLR2 and TLR4. J Immunol 181:2103–2110
Mack JA, Feldman RJ, Itano N, Kimata K, Lauer M, Hascall VC, Maytin EV (2011) Enhanced inflammation and accelerated wound closure following tetraphorbol ester application or full-thickness wounding in mice lacking hyaluronan synthases Has1 and Has3. J Invest Dermatol (in press)
Savage K, Swann DA (1985) A comparison of glycosaminoglycan synthesis by human fibroblasts from normal skin, normal scar, and hypertrophic scar. J Invest Dermatol 84:521–526
Swann DA, Garg HG, Jung W, Hermann H (1985) Studies on human scar tissue proteoglycans. J Invest Dermatol 84:527–531
Jokela TA, Lindgren A, Rilla K, Maytin E, Hascall VC, Tammi RH, Tammi MI (2008) Induction of hyaluronan cables and monocyte adherence in epidermal keratinocytes. Connect Tissue Res 49:115–119
West DC, Shaw DM, Lorenz P, Adzick NS, Longaker MT (1997) Fibrotic healing of adult and late gestation fetal wounds correlates with increased hyaluronidase activity and removal of hyaluronan. IntJ Biochem Cell Biol 29:201–210
Monslow J, Sato N, Mack JA, Maytin EV (2009) Wounding-induced synthesis of hyaluronic acid in organotypic epidermal cultures requires the release of heparin-binding egf and activation of the EGFR. J Invest Dermatol 129:2046–2058
Lorenz HP, Lin RY, Longaker MT, Whitby DJ, Adzick NS (1995) The fetal fibroblast: the effector cell of scarless fetal skin repair. Plast Reconstr Surg 96:1251–1259
Hsu FY, Hung YS, Liou HM, Shen CH (2010) Electrospun hyaluronate-collagen nanofibrous matrix and the effects of varying the concentration of hyaluronate on the characteristics of foreskin fibroblast cells. Acta Biomater 6:2140–2147
Franz S, Rammelt S, Scharnweber D, Simon JC (2011) Immune responses to implants—a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32:6692–6709
Wiegand C, Schonfelder U, Abel M, Ruth P, Kaatz M, Hipler UC (2010) Protease and pro-inflammatory cytokine concentrations are elevated in chronic compared to acute wounds and can be modulated by collagen type I in vitro. Arch Dermatol Res 302:419–428
Moseley R, Hilton JR, Waddington RJ, Harding KG, Stephens P, Thomas DW (2004) Comparison of oxidative stress biomarker profiles between acute and chronic wound environments. Wound Repair Regen 12:419–429
Vallieres M, du Souich P (2010) Modulation of inflammation by chondroitin sulfate. Osteoarthritis Cartilage 18(Suppl 1):S1–S6
Day AJ, de la Motte CA (2005) Hyaluronan cross-linking: a protective mechanism in inflammation? Trends Immunol 26:637–643
Chen WY, Abatangelo G (1999) Functions of hyaluronan in wound repair. Wound Repair Regen 7:79–89
Foschi D, Castoldi L, Radaelli E, Abelli P, Calderini G, Rastrelli A, Mariscotti C, Marazzi M, Trabucchi E (1990) Hyaluronic acid prevents oxygen free-radical damage to granulation tissue: a study in rats. Int J Tissue React 12:333–339
Orlandi RR, Shu XZ, McGill L, Petersen E, Prestwich GD (2007) Structural variations in a single hyaluronan derivative significantly alter wound-healing effects in the rabbit maxillary sinus. Laryngoscope 117:1288–1295
Scuderi N, Anniboletti T, Carlesimo B, Onesti MG (2009) Clinical application of autologous three-cellular cultured skin substitutes based on esterified hyaluronic acid scaffold: our experience. In Vivo 23:991–1003
Dieckmann C, Renner R, Milkova L, Simon JC (2010) Regenerative medicine in dermatology: biomaterials, tissue engineering, stem cells, gene transfer and beyond. Exp Dermatol 19:697–706
Lam PK, Chan ES, To EW, Lau CH, Yen SC, King WW (1999) Development and evaluation of a new composite Laserskin graft. J Trauma 47:918–922
Wang TW, Sun JS, Wu HC, Tsuang YH, Wang WH, Lin FH (2006) The effect of gelatin-chondroitin sulfate-hyaluronic acid skin substitute on wound healing in SCID mice. Biomaterials 27:5689–5697
Gama CI, Hsieh-Wilson LC (2005) Chemical approaches to deciphering the glycosaminoglycan code. Curr Opin Chem Biol 9:609–619
Gama CI, Tully SE, Sotogaku N, Clark PM, Rawat M, Vaidehi N, Goddard WA 3rd, Nishi A, Hsieh-Wilson LC (2006) Sulfation patterns of glycosaminoglycans encode molecular recognition and activity. Nat Chem Biol 2:467–473
Nemeth-Csoka M, Kajtar M, Kajtar J (1977) The role of sulphation of glycosaminoglycans in their structural and functional characteristics. Connect Tissue Res 5:1–6
Funding sources
This study is supported by grants from Deutsche Forschungsgemeinschaft Transregio 67 (projects B1, B2, B3, and B4).
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salbach, J., Rachner, T.D., Rauner, M. et al. Regenerative potential of glycosaminoglycans for skin and bone. J Mol Med 90, 625–635 (2012). https://doi.org/10.1007/s00109-011-0843-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-011-0843-2