Abstract
Aims/hypothesis
Linagliptin has protective effects on the retinal neurovascular unit but, in proliferative retinopathy, dipeptidyl peptidase 4 (DPP-4) inhibition could be detrimental. The aim of this study was to assess the effect of linagliptin on ischaemia-induced neovascularisation of the retina.
Methods
C57BL/6J and glucagon-like peptide 1 (GLP-1) receptor (Glp1r)−/− mice were subjected to a model of oxygen-induced retinopathy (OIR). Both strains were subcutaneously treated with linagliptin from postnatal days 12 to 16. Non-injected OIR and non-exposed mice served as controls. Capillary proliferations and systemic levels of active GLP-1 were quantified. The effects of linagliptin on vascular endothelial growth factor (VEGF)-induced downstream signalling were assessed in human umbilical vein endothelial cells (HUVECs) using western blot for retinal phosphorylated extracellular signal-regulated kinase (ERK)1/2 and retinal gene expression analyses.
Results
Linagliptin treatment led to an increase in active GLP-1 and a decreased number of neovascular nuclei in OIR mice vs controls (−30%, p < 0.05). As the reduction in neovascularisation was similar in both C57BL/6J and Glp1r−/− mice, the anti-angiogenic effects of linagliptin were independent of GLP-1R status. The expression of Vegf (also known as Vegfa) and Hif1a was increased in C57BL/6J OIR mice upon linagliptin treatment (three- vs 1.5-fold, p < 0.05, p < 0.01, respectively). In HUVECs, linagliptin inhibited VEGF-induced increases in mitogen-activated protein kinase (MAPK)/ERK (−67%, p < 0.001) and MAPK/c-Jun N-terminal kinase (JNK) (−13%, p < 0.05) pathway activities. In the retinas of C57BL/6J mice, p-ERK1/2 levels were significantly reduced upon linagliptin treatment (−47%, p < 0.05).
Conclusions/interpretation
Systemic treatment with linagliptin demonstrated GLP-1R-independent anti-angiogenic effects mediated by an inhibition of VEGF receptor downstream signalling. The specific effects of linagliptin on diabetic retinopathy are of potential benefit for individuals with diabetes, independent of metabolic effects.
Similar content being viewed by others

Introduction
Diabetic retinopathy is a major burden for health systems in industrialised countries, and has substantial personal and financial implications [1, 2]. The early phases of diabetic retinopathy are defined by vasoregressive processes aggravated by retinal inflammation and gliosis, which result in progressive retinal ischaemia [2]. The hypoxic retinal areas express a variety of cytokines and growth factors to maintain neuroretinal function and promote the revascularisation of ischaemic areas [3]. The most important signalling pathway during the proliferative diabetic retinopathy stages is the hypoxia-inducible factor 1α (HIF1A)–vascular endothelial growth factor (VEGF) pathway [2, 3]. Stabilisation of HIF1A by low intracellular oxygen levels leads to the nuclear translocation of HIF1A, resulting in the upregulation of proangiogenic factors such as VEGF [4]. As the hypoxic areas are unevenly distributed throughout the retina, however, no stable gradient of VEGF can be maintained, resulting in an undirected angiogenic response [2, 5]. These neovascularisations are immature and unstable, which results in a high probability of intravitreal bleeding of the neovascularisations, ultimately leading to blindness [6].
Inhibitors of dipeptidyl peptidase 4 (DPP-4) are approved for the treatment of type 2 diabetes and have shown a variety of beneficial effects beyond reducing hyperglycaemia [7, 8]. DPP-4 inhibitors have been demonstrated to reduce vascular complications of diabetes, such as atherosclerosis and myocardial infarction, by mitigating endothelial inflammation [9]. In experimental models of early-stage diabetic retinopathy, DPP-4 inhibition has shown conflicting results. Whereas linagliptin has been shown to mediate vasoprotective and anti-inflammatory effects in animals with streptozotocin-induced diabetes [10], DPP-4 inhibition with sitagliptin and diprotin A has demonstrated detrimental effects on the retinal vasculature, with increased permeability via Src and vascular endothelial-cadherin phosphorylation [11]. These contradictory results provide the possibility that the effects of DPP-4 inhibitors are not only mediated by the increase in active glucagon-like peptide (GLP)-1 levels and their interaction with the GLP-1 receptor (GLP-1R), but that the effects on the retinal vasculature are influenced, at least in part, by substance-specific interactions.
DPP-4 does not only cleave the incretin hormone GLP-1, but also several proangiogenic factors such as high-mobility group box 1 (HMGB-1) and stromal cell-derived factor 1 α (SDF-1α) [8, 12]. In proliferative retinopathies, SDF-1α and VEGF act synergistically on neovascularisation through a partial overlap of downstream signalling pathways [13,14,15]. Both SDF-1α/CXCR4 and VEGF/VEGF receptor (VEGFR) activity are necessary to develop proliferative retinopathy, and an increase in SDF-1α/CXCR4 activity alone is sufficient to induce retinal neovascularisation [16]. The increase in vascular permeability upon diprotin A and sitagliptin treatment is at least partially mediated by SDF-1α [11]. In contrast, upon linagliptin treatment, neither an increase in SDF-1α levels nor a proangiogenic response was observed in streptozotocin-induced diabetic rats [10]. In the oxygen-induced retinopathy (OIR) model, a model of retinal neovascularisation with similar underlying mechanisms as proliferative diabetic retinopathy, treatment with diprotin A has not only been reported to induce aggravated permeability, but also to cause a strong proangiogenic response resulting in complete revascularisation of the avascular zone at postnatal day 17 [11]. The differences in SDF-1α levels upon treatment with various DPP-4 inhibitors are probably due to differences in inhibitory activity towards the DPP-4 structural homologues DPP-2, DPP-8 and DPP-9 [17]. These homologues show enzymatic activity and participate to varying degrees in the cleavage of SDF-1α and HMGB-1 [18]. Compared with diprotin A and sitagliptin, linagliptin shows a significantly higher specificity towards DPP-4 over DPP-8/9, which might explain the differences in angiogenic response between the substances, but the effects of linagliptin on proliferative retinopathy have not previously been tested [19].
The aim of this study was to investigate the effects of linagliptin on angiogenesis in the retina. In addition, to assess the role of GLP-1R, we compared the influence of linagliptin on retinal neovascularisation in both C57BL/6J and Glp1r−/− mice.
Methods
Animals
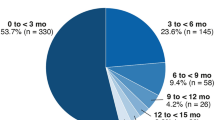
The care and experimental use of all animals in the study were in accordance with EC directive 2010/63/EU and in compliance with the Association for Research in Vision and Ophthalmology statement. All animal experiments were approved by the local ethics committee (Regierungspräsidium Karlsruhe, Karlsruhe, Germany). Mice were kept in a specified pathogen-free environment in 12 h light–dark cycles with free access to food and water. Male C57BL/6J mice, purchased from Charles River (Wilmington, MA, USA) and homozygous Glp1r−/− mice (Glp1rtm1Ddr), kindly provided by Boehringer Ingelheim, were used for the OIR model (Boehringer Ingelheim, Biberach an der Riß, Germany) [20]. Each mouse strain was divided into three groups: mice without OIR as controls; mice with OIR; and mice with OIR treated with subcutaneous linagliptin (Boehringer Ingelheim) from postnatal day 12 to 16 at a concentration of 10 mg/kg body weight (OIR + Lina). Animals of each litter were randomly numbered and numbers equally assigned from top to bottom to OIR and OIR + Lina. Every third litter was selected as control group without subjection to the OIR model. At postnatal days 12 and 17, both eyes of mice in randomly selected litters were isolated during isoflurane anaesthesia and the mice killed by cervical dislocation. The eyes were fixed in 4% (vol./vol.) formalin for analysis of neovascularisation or stored at −80°C for gene expression analysis. Plasma was obtained for the determination of active GLP-1 as an indicator of DPP-4 inhibition by linagliptin.
OIR model
Glp1r−/− and C57BL/6J mice were investigated for quantification of preretinal neovascularisation using the established OIR model for mice in periodic acid Schiff-stained paraffin sections [21]. In brief, newborn mouse litters were exposed from postnatal day 7 until postnatal day 12 in an incubation chamber with 75% (vol./vol.) oxygen and then returned to room air until postnatal day 17. Linagliptin was administrated from postnatal day 12 to postnatal day 16. OIR litters consisted of OIR control mice and linagliptin-treated animals, randomly assigned to the treatment group. Litters kept in room air for the entire time until postnatal day 17 served as controls.
Determination of the avascular zone
To evaluate vasoregression, eyes from C57BL/6 and Glp1r−/− mice at OIR postnatal day 12 were submitted to immunofluorescence staining with collagen IV (1:100; Acris, Herford, Germany) to visualise the vessel net in the superficial layer and to lectin-FITC (1:50; Sigma-Aldrich, Munich, Germany) to visualise capillaries in the superficial and deep layers. After overnight incubation, the following secondary antibody for collagen IV was used: swine anti-rabbit tetramethylrhodamine (1:50; Dako Cytomation, Hamburg, Germany). The avascular zone was measured using Cell-F imaging software (Olympus Opticals, Hamburg, Germany) at ×2 magnification.
Experimenters were blinded for the quantification of neovascularisations and avascular zones.
Determination of active GLP-1
Active GLP-1 concentrations (GLP-1 [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] amide and GLP-1 [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37]) were determined in the plasma of the animals at the end of the study using commercially available ELISAs (K150JVC-1 and K150JWC-1, Meso Scale Discovery, Gaithersburg, MD, USA).
Receptor tyrosine kinase signalling reporter assay
Human umbilical vein endothelial cells (HUVECs; Thermo Fisher Scientific, Weiterstadt, Germany; authenticated and confirmed mycoplasma-negative by the supplier) were cultured to 90% confluence. The RTK Signaling 10-Pathway Reporter Array (Qiagen, Hilden, Germany) was used to measure the activity of the mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK), MAPK/c-Jun N-terminal kinase (JNK), phosphoinositide 3-kinase (PI3K)/Akt and NFκB pathways according to the manufacturer’s instructions. In brief, cells were reversely transfected with the corresponding DNA constructs using the Attractene transfection reagent (Qiagen) for 24 h in OPTI-MEM (Thermo Fisher Scientific). After transfection, cells were stimulated with 10 ng/ml VEGF (Sigma-Aldrich, Munich, Germany) with or without 50 nmol/l linagliptin (Boehringer Ingelheim) for 24 h. Firefly and Renilla luciferase signals were detected using a common microplate reader (Spark, Tecan Trading, Männedorf, Switzerland) using a dual-luciferase assay (Promega, Mannheim, Germany) according to the manufacturer’s protocol.
Western blot for p-ERK1/2, ERK1/2 and p-VEGFR2
The isolated retina was homogenised in 0.1% (wt/vol.) SDS lysis buffer and the protein concentration was determined using the Bradford assay (Bio-Rad, Munich, Germany). Samples were separated in a 4–20% (wt/vol.) gradient TGX Gel (Bio-Rad) and immunoblotted to a polyvinylidene difluoride membrane (Bio-Rad). Unspecific binding was blocked by incubation with 5% (wt/vol.) non-fat dry milk in Tris-buffered saline containing 0.1% (vol./vol.) Tween (Sigma-Aldrich, Darmstadt, Germany), followed by overnight incubation at 4°C with the antibodies mouse anti-mouse p-ERK1/p-ERK2 (1:10,000; Abcam, Cambridge, UK), rabbit anti-mouse ERK1/ERK2 (1:1500; Abcam), rabbit anti-mouse p-Tyr1175VEGFR2 (1:1300; Cell Signaling, Frankfurt, Germany) or rabbit anti-mouse β-tubulin (1:500; Abcam). For detection, horseradish-peroxidase conjugated antibodies against mouse for p-ERK1/p-ERK2 (1:1000; Dako Cytomation) and against rabbit for ERK1/ERK2 (1:2000, Cell Signaling), p-VEGFR (1:2000; Cell Signaling) and tubulin (1:3000; Dako Cytomation) were used. Antibodies were validated by the manufacturer and in previous studies. Immunoreactive bands were visualised by incubation in chemiluminescence reagent (PerkinElmer, Boston, MA, USA) and signals were detected using the Fusion SL (VWR, Darmstadt, Germany). Integrated densities were measured using ImageJ software v 1.50i [22].
Gene expression analysis
Retinal RNA was isolated and homogenised in TRIzol reagent (Invitrogen, Karlsruhe, Germany). RNA was reverse transcribed using the QuantiTect Reverse Transcription kit (Qiagen) and subjected to quantitative (q)PCR analysis using hydrolysis probes (TaqMan probes, Applied Biosystems, Weiterstadt, Germany). Gene expression was analysed by the comparative ΔΔCq method using Actb and Gapdh as reference genes. All primers and probes were purchased from Applied Biosystems (see electronic supplementary material [ESM] Table 1 for details).
Measurement of total SDF-1α
Systemic total SDF-1α was measured in EDTA plasma using a standard Luminex assay (Natural and Medical Sciences Institute, University of Tübingen, Tübingen, Germany). The protocol uses overnight incubation on Millipore filter plates (Merck Millipore, Darmstadt, Germany) and beads to measure total SDF-1α.
cAMP determination
For cAMP measurement, eyes for retinal explants from adult C57BL/6J and Glp1r−/− mice were obtained under deep anaesthesia and immediately transferred to OPTI-MEM (Thermo Fisher Scientific) containing IBMX (3-isobutyl-1-methylxanthine; Sigma-Aldrich, Munich, Germany). The left retinal explant was treated with GLP-1 (7-36) amide (Bachem, Bubendorf, Switzerland) and lixisenatide (Sanofi, Frankfurt, Germany) as binding ligands for GLP-1R. The right retinal explant served as an untreated control. After explant lysis, cAMP was measured using a cAMP direct fluorimetric immunoassay kit (Abcam) according to the manufacturer’s instructions.
Statistical analysis
Quantification of neovascular nuclei, avascular zones and active GLP1 has been performed once with the number of animals stated in the figure legends. The receptor tyrosine kinase signalling reporter assay has been performed as four-time quantified duplicates, with the mean of two simultaneously measured duplicates for each group being n = 1 of 4. Western blots have been performed twice with the experiment showing the maximum spread of grey values being quantified. Gene expression analysis has been performed in duplicate. Data are presented as means ± SD. Differences between groups were analysed using ANOVA with the Bonferroni post hoc method for multiple comparisons. Statistical outliers were identified using the ROUT method with Q = 1%. Statistical analyses were performed using GraphPad Prism v6.01 (GraphPad Software, San Diego, CA, USA). For all comparisons, p < 0.05 was considered statistically significant.
Results
Elevated levels of systemic active GLP-1 upon linagliptin treatment
First, the efficacy of systemic treatment with linagliptin was analysed. For that, the systemic levels of active GLP-1, as a proposed acting mechanism of DPP-4 inhibition, were measured in the plasma of C57BL/6J and Glp1r−/− mice. In OIR mice, the levels of active GLP-1 were slightly increased in both strains, but not to statistical significance (control vs OIR: C57BL/6J: 0.44 ± 0.22 vs 1.56 ± 0.56 pg/ml, p = 0.880; Glp1r−/−: 0.51 ± 0.27 vs 7.30 ± 7.54 pg/ml, p = 0.414; Fig. 1). However, treatment with linagliptin resulted in a significant elevation of active GLP-1 in the plasma of both C57BL/6J and Glp1r−/− mice (C57BL/6J: 17.54 ± 6.17 pg/ml, p < 0.001 vs OIR; Glp1r−/−: 25.50 ± 11.51 pg/ml, p < 0.001 vs OIR; Fig. 1). The elevation appeared to be more pronounced in C57BL/6J compared with Glp1r−/− mice due to higher levels of active GLP-1 in the OIR model. This effect was, however, statistically non-significant (C57BL/6J OIR vs Glp1r−/− OIR, p = 0.621; Fig. 1).
The concentration of active GLP-1 in plasma, representing the effectiveness of DPP-4 inhibition by linagliptin in (a) C57BL/6J and (b) Glp1r−/− mice. Data are expressed as means ± SD for six, eight and 12 C57BL/6J mice, and four, ten and nine Glp1r−/− mice (both Ctrl p17, OIR p17 and OIR p17 + Lina, respectively). Ctrl, control; p17, postnatal day 17. ***p < 0.001 vs OIR
Linagliptin treatment mitigated neovascularisation
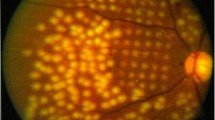
Next, we examined the effects of linagliptin on the retinal vasculature (Fig. 2a). Systemic treatment with linagliptin resulted in a reduction in preretinal, intravitreal neovascular nuclei by 30% (OIR vs OIR + Lina: 55 ± 21 vs 38 ± 10 nuclei, p = 0.015; Fig. 2b). To determine whether the anti-angiogenic effects were dependent on GLP-1R signalling, we used Glp1r−/− mice in the OIR model. Untreated Glp1r−/− animals did not show any significant differences in response to the OIR model, as the avascular zone and neovascular nuclei were of similar sizes (C57BL/6J vs Glp1r−/−: avascular zone: 5.57 ± 0.98 vs 4.67 ± 0.82 mm2, p = 0.101; neovascular nuclei: 55 ± 21 vs 42 ± 13 nuclei, p = 0.155; Fig. 2b, c; electronic supplementary material [ESM] Fig. 1a). In the absence of Glp1r expression (ESM Fig. 1b), systemic treatment with linagliptin led to a reduction in the number of neovascular nuclei by 30% (OIR vs OIR + Lina: 42 ± 13 vs 27 ± 12 nuclei, p = 0.0171; Fig. 2c), similar to in C57BL/6J mice.
Retinal neovascularisations growing into the vitreous body in C57BL/6J and Glp1r−/− mice at OIR postnatal day 17 (p17). (a) Representative images showing neovascular nuclei (arrowheads). Scale bars, 200 μm. Quantification of neovascular nuclei in C57BL/6J (b) and Glp1r−/− (c) mice. Data are expressed as means ± SD for 11 and 15 C57BL/6J mice, and ten and nine Glp1r−/− mice (both OIR p17 and OIR p17 + Lina, respectively). *p < 0.05
Increased expression of proangiogenic genes upon linagliptin treatment
To assess the impact of DPP-4 inhibition on angiogenesis and inflammation, we performed qPCRs for proangiogenic and proinflammatory genes. In C57BL/6J mice, the OIR model led to an expected two- and fourfold increase in the expression of the proangiogenic Vegf (also known as Vegfa) and Angpt2, respectively (Vegf: 2.1 ± 0.2-fold, p = 0.019; Angpt2: 4.8 ± 2.2-fold; p < 0.001; Fig. 3a, b). The expression of Hif1a was slightly but not significantly reduced in C57BL/6J OIR mice (0.7 ± 0.1-fold, p = 0.289; Fig. 3f). Furthermore, the OIR model led to a significant increase in the proinflammatory factors Tnfa (also known as Tnf) (5.0 ± 1.4-fold, p = 0.005; Fig. 3c) and Il1b (8.7 ± 3.7-fold, p < 0.001; Fig. 3e), as well as in the neuroprotective but also proangiogenic Epo (13.7 ± 3.5-fold, p < 0.001; Fig. 3d). Systemic treatment with linagliptin showed no significant effects on the expression of Angpt2, Tnfa, Epo or Il1b (Fig. 3b–e). However, the expression of Vegf was significantly increased in linagliptin-treated C57BL/6J mice (3.1 ± 1.0-fold of control; p = 0.016 vs OIR; Fig. 3a). Consistent with the reduction in neovascularisation, Hif1a expression was significantly increased upon treatment with linagliptin (1.4 ± 0.5-fold of control; p = 0.005 vs OIR; Fig. 3f).
Relative retinal expression of (a) Vegf, (b) Angpt2, (c) Tnfa, (d) Epo, (e) Il1b and (f) Hif1a in C57BL/6J mice. Data are expressed as means ± SD for six mice normalised to control (Ctrl) postnatal day 17 (p17) for all, except for five mice for Tnfa Ctrl p17, Il1b Ctrl p17 and Il1b OIR p17 + Lina. *p < 0.05, **p < 0.01, ***p < 0.001
Induction of Vegf shows systemic GLP-1R dependency
To differentiate between GLP-1R-dependent and -independent gene expression changes upon linagliptin treatment, expression of the same genes was determined in Glp1r−/− mice. The expression of proangiogenic genes was similar between C57BL/6J and Glp1r−/− mice under either control conditions or after subjection to the OIR model (Figs 3a–f and 4a–f). OIR induced similar upregulations of Vegf, Angpt2, Epo and Il1b in Glp1r−/− to the C57BL/6J mice (Fig. 4a, b, d, e). The expression of Hif1a was downregulated similarly to in C57BL/6J mice (Fig. 4f). This regulation was, in contrast to C57BL/6J mice, significant in Glp1r−/− mice, due to the absence of regulation upon linagliptin treatment. In contrast, the expression of Tnfa was not significantly upregulated in Glp1r−/− mice subjected to the OIR model (1.7 ± 0.7- vs 3.0 ± 0.4-fold of C57BL/6J control; control vs OIR, p = 0.082; Fig. 4c). Upon treatment with linagliptin, Glp1r−/− mice showed no significant regulation of Vegf, which was observed in C57BL/6J mice (2.2 ± 0.5- vs 2.1 ± 0.4-fold of C57BL/6J control; OIR vs OIR + Lina, p = 0.812; Fig. 4a). The expression of Il1b was significantly reduced in linagliptin-treated Glp1r−/− animals (9.8 ± 1.1- vs 6.0 ± 2.3-fold of C57BL/6J control; OIR vs OIR + Lina, p = 0.005; Fig. 4e). This effect was also observed in C57BL/6J mice, but was not statistically significant (8.7 ± 3.7- vs 5.3 ± 1.7-fold of C57BL/6J control; OIR vs OIR + Lina, p = 0.080; Fig. 3e).
Relative retinal expression of (a) Vegf, (b) Angpt2, (c) Tnfa, (d) Epo, (e) Il1b and (f) Hif1a in Glp1r−/− mice. Data are expressed as means ± SD for six mice normalised to C57BL/6J control (Ctrl) postnatal day 17 (p17) for all, except for five mice for Vegf OIR p17, Angpt2 OIR p17, Epo OIR p17 and Il1b OIR p17 + Lina; and four mice for Tnfa OIR p17 and Il1b OIR p17. *p < 0.05, **p < 0.01, ***p < 0.001
Linagliptin prevented VEGF-induced activation of MAPK
The anti-angiogenic effects of linagliptin in the presence of unchanged or even increased levels of Vegf mRNA suggest an interference of linagliptin with the downstream signalling of VEGFR. In order to identify effector mechanisms of linagliptin’s anti-angiogenic effects, HUVECs were stimulated with VEGF in the presence or absence of linagliptin (50 nmol/l) and the activities of different receptor tyrosine kinase-dependent pathways were analysed. VEGF stimulation led to an increase in MAPK/ERK activity, which was prevented by linagliptin with a reduction in activity of −67% (2.67 ± 0.30- vs 0.87 ± 0.11-fold of control; VEGF vs VEGF + Lina, p < 0.001; Fig. 5a). Furthermore, VEGF-induced activation of the MAPK/JNK pathway was mitigated by −13% in linagliptin treated cells (1.48 ± 0.13- vs 1.29 ± 0.18-fold of control; control vs VEGF, p = 0.024; control vs VEGF + Lina, p = 0.203; Fig. 5b). The activity of the PI3K/Akt pathway was not affected by VEGF stimulation, but treatment with linagliptin led to a decrease compared with control conditions (0.88 ± 0.12- vs 0.66 ± 0.16-fold of control; control vs VEGF + Lina, p = 0.0117; Fig. 5c). NFκB activity showed an increasing trend upon VEGF stimulation, which was prevented by linagliptin, but the effect remained statistically not significant (1.30 ± 0.36- vs 0.93 ± 0.29-fold of control; VEGF vs VEGF + Lina, p = 0.201; Fig. 5d).
Receptor tyrosine kinase signalling in HUVECs treated with VEGF and VEGF + linagliptin for (a) MAPK/ERK (control and VEGF, n = 4; VEGF + Lina, n = 3), (b) MAPK/JNK (control and VEGF, n = 4; VEGF + Lina, n = 3), (c) PI3K/Akt (n = 4) and (d) NFκB (control and VEGF + Lina, n = 4; VEGF, n = 3). p-ERK signalling in the retina from (e) C57BL/6J and (f) Glp1r−/− mice (all n = 5) with representative images (g, h). Data are expressed as means ± SD. Ctrl, control; p17, postnatal day 17. *p < 0.05, ***p < 0.001
To confirm the in vitro observations in the retinas of C57BL/6J and Glp1r−/− mice, we performed western blots for the phosphorylation of ERK1/2, which was the most affected pathway in the cell culture experiments. In line with the in vitro results, the phosphorylation of ERK1/2 was significantly increased in C57BL/6J OIR mice, and this increase was prevented by linagliptin treatment with a reduction of −47% (p-ERK/ERK1/2 ratio of 0.30 ± 0.00 vs 0.80 ± 0.45 vs 0.42 ± 0.16, control vs OIR vs OIR + Lina; control vs OIR, p = 0.044; control vs OIR + Lina, p = 0.881; Fig. 5e, g). In Glp1r−/− mice, however, the induction of p-ERK1/2 showed an insignificant positive trend. Consequently, linagliptin treatment did not lead to a significant reduction in ERK1/2 phosphorylation (0.34 ± 0.11 vs 0.48 ± 0.24 vs 0.46 ± 0.15, control vs OIR vs OIR + Lina; control vs OIR, p = 0.548; OIR vs OIR + Lina, p = 0.997; Fig. 5f, h).
To investigate if the inhibition of ERK1/2 phosphorylation by linagliptin was mediated by an inhibition of VEGFR2 phosphorylation, we performed western blots for the phosphorylation of Tyr1175 of VEGFR2, which mediates activation of the MAPK/ERK signalling pathway. In mice subjected to the OIR model, the amount of p-VEGFR2 was significantly increased in both strains (p-VEGFR2/tubulin ratio, control vs OIR: C57BL/6J, 0.66 ± 0.03 vs 0.71 ± 0.02, p = 0.041; Glp1r−/−, 0.48 ± 0.01 vs 0.57 ± 0.04, p = 0.048; Fig. 6a, b). The amount of p-VEGFR2 was not affected by linagliptin treatment in either model (OIR vs OIR + Lina: C57BL/6J, 0.71 ± 0.02 vs 0.71 ± 0.03, p = 0.996; Glp1r−/−, 0.57 ± 0.04 vs 0.61 ± 0.06, p = 0.369; Fig. 6a, b).
Absence of relevant retinal GLP-1R signalling
To discriminate between systemic and retinal effects of DPP-4 inhibition and GLP-1R status, we quantified the systemic levels of SDF-1α and the effect on retinal GLP-1R signalling capacity. SDF-1α levels were measured in the plasma of C57BL/6J and Glp1r−/− mice to estimate the impact of SDF-1α on the retinal angiogenic balance. In OIR animals, the levels of total SDF-1α were not affected in either C57BL/6J or Glp1r−/− mice. Upon treatment with linagliptin, however, the levels of SDF-1α were significantly higher in C57BL/6J mice only (OIR vs OIR + Lina: C57BL/6J, 623.8 ± 315.7 vs 2105.0 ± 895.3 pg/ml, p = 0.002; Glp1r−/−, 1038.0 ± 628.2 vs 1871.0 ± 643.7 pg/ml, p = 0.085; Fig. 7a, b). As the expression levels of retinal Glp1r were low in C57BL/6J mice, we determined the overall capacity of retinal GLP-1R signalling by quantifying GLP-1R-induced cAMP production in retinal explants. To discriminate between GLP-1R and unspecific cAMP production, Glp1r−/− mice without any retinal Glp1r expression (ESM Fig. 1b) served as an additional control. Upon dual stimulation with active GLP-1 and a GLP-1R agonist, slight increases in retinal cAMP were observed in retinas of both C57BL/6J and Glp1r−/− mice. These increases were statistically significant only in C57BL/6J mice (1.37 ± 0.05-fold of untreated control, p = 0.040; Fig. 7c). However, as the magnitude of increased cAMP was similar in both strains, these increases were most likely due to GLP-1R-independent, direct effects of the dual stimulation (C57BL/6J vs Glp1r−/−: 1.37 ± 0.05- vs 1.42 ± 0.18-fold of untreated control, p = 0.996; Fig. 7c).
Plasma levels of total SDF-1α in (a) C57BL/6J and (b) Glp1r−/− mice. Data are expressed as means ± SD for six mice. **p < 0.01. (c) cAMP in retinal explants from C57BL/6J (white bars) and Glp1r−/− (black bars) mice treated with GLP-1 (7–36) amide and lixisenatide (GLP-1R agonists). Data are expressed as means ± SD for three explants. Ctrl, control; p17, postnatal day 17. *p < 0.05
Discussion
In this study, we have demonstrated that the DPP-4 inhibitor linagliptin has anti-angiogenic effects in a mouse model of OIR, which are independent of GLP-1R signalling. The anti-angiogenic properties of linagliptin are mediated by inhibition of the VEGF-induced MAPK/ERK pathway in endothelial cells.
VEGF-induced VEGFR2 autophosphorylation and subsequent receptor tyrosine kinase activity have been described to be mandatory for the proangiogenic effects of VEGF [23, 24]. The increase in VEGF expression in the OIR model is induced by increased translational activity of HIF1A in the avascular retinal centre in a hypoxia-dependent manner [25,26,27]. VEGFR-induced activation of MAPK signalling pathways is a key feature in VEGF-mediated angiogenesis, which in our study was inhibited by linagliptin in endothelial cells [26,27,28]. The activation of MAPK is predominantly mediated by phosphorylation of Tyr1175, which was not changed upon linagliptin treatment in the OIR mice analysed in this study [27]. This indicates that linagliptin either inhibits the interaction of the phosphorylated tyrosine sites with their transducers, phosphoinositide phospholipase C γ (PLCg) and p38/MAPK, or interferes downstream in the signalling cascades [29]. The decrease in PI3K/Akt activity in HUVECs in the presence of linagliptin and in the absence of a significant activation by VEGF in the current study suggests inhibition of phosphorylation site activities, as PI3K/Akt activation is induced by the interaction of pTyr1175 and SH2 domain containing adaptor protein B (SHB)/SHC adaptor protein 2 (SCK) [29, 30]. Inhibitory effects on these pathways, especially MAPK/ERK activity, has previously been demonstrated in fibroblasts, where linagliptin led to a decrease in p-ERK1/2 upon glucose stimulation [31].
The inhibition of VEGFR2 downstream signalling by linagliptin is in accordance with the gene expression results. The increased expression of Vegf in linagliptin-treated animals is induced by the slower revascularisation of the hypoxic avascular centre, indicated by the lower number of neovascular nuclei [21, 32]. The absence of significant Vegf regulation in Glp1r−/− mice can be explained by the lower amount of angiogenic activity observed in the Glp1r−/− mice subjected to OIR. Linagliptin was associated with a minor decrease in NFκB signalling in endothelial cells, consistent with an anti-inflammatory effect on the vasculature that has already been described [9, 33]. However, despite its anti-inflammatory properties in other retinopathy models, in this study linagliptin showed no effect on major proinflammatory cytokines in the OIR model [10]. Anti-inflammatory effects are associated with proangiogenic responses in the retina, as key proinflammatory pathways can inhibit the activity of VEGF-induced VEGFR signalling, as has been described elsewhere in detail for the semaphorin 3A (SEMA3A)–neuropilin 1 (NRP1) axis [34,35,36].
Minor differences between wild-type and Glp1r−/− animals with regard to vasoregression, neovascularisation and retinal gene expression in the OIR model are indicative of GLP-1R-mediated effects in the process of pathological angiogenesis. However, as we observed only a small magnitude of GLP-1R-dependent signalling in the retina and as the expression of GLP-1R is present only at very low levels, these effects have to be regulated indirectly by systemic GLP-1R-dependent signalling pathways [37]. Regardless of retinal GLP-1R expression, the effects of DPP-4 inhibition on the angiogenic response were similar in C57BL/6J and Glp1r−/− mice, which is consistent with recently published observations [38].
The increase in active GLP-1 upon linagliptin treatment is consistent with significant inhibition of DPP-4 enzymatic activity, as has previously been demonstrated in a rat model of diabetic retinopathy [10]. DPP-4 has a broad spectrum of substrates, including the proangiogenic SDF-1α and HMGB-1 [8, 12]. Our study showed that the levels of total SDF-1α were unaffected by DPP-4 inhibition in Glp1r−/− mice, but were increased by linagliptin in wild-type mice. Because the assay does not discriminate between active and total SDF-1α, this difference may reflect GLP-1R-dependent mechanisms in SDF-1α synthesis and metabolism. Regardless of SDF-1α, linagliptin overall demonstrated anti-angiogenic effects in the OIR model, limiting the impact of systemic SDF-1α on retinal angiogenesis. As the observed anti-angiogenic effect of linagliptin was mediated by inhibition of ERK1/2 phosphorylation, and both VEGF/VEGFR and SDF-1α/CXCR4 can exert their angiogenic properties via MAPK/ERK signalling, we cannot exclude inhibitory effects of linagliptin on SDF-1α/CXCR4-mediated ERK1/2 phosphorylation [15]. But as the inhibition of ERK1/2 phosphorylation was stronger in C57BL/6J mice, in which the levels of SDF-1α were significantly higher compared with Glp1r−/− mice (in which the levels of SDF-1α were unchanged), the effects of systemic SDF-1α on retinal MAPK/ERK signalling were probably negligible. These results are in accordance with those of a previous study, in which systemic treatment with linagliptin, associated with vasoprotection, did not lead to a significant increase in SDF-1α or HMGB-1 levels [10].
In summary, we have demonstrated anti-angiogenic effects of linagliptin treatment in the OIR model independent of GLP-1R signalling. We have shown that this effect is mediated in vitro by inhibition of VEGFR downstream signalling, which might also apply in retinal endothelial cells. Our data point to a possible mechanism involving the interactions of p-Tyr1175 and p-Tyr1214 with their respective transducing factors. However, the exact mechanism by which linagliptin inhibits these interactions remains unknown. Furthermore, the extent to which the anti-oxidant effects of linagliptin play a role in this process was not investigated in this study [39]. The interactions of linagliptin with angiopoietin-2 signalling were not addressed, but the assessment of angiopoietin-2 activity would be of great consequence, as linagliptin acts on vasoregression and angiogenesis and angiopoietin-2 is a key factor in both processes [10, 40]. Combining these findings with those from previous studies, we conclude that linagliptin has beneficial effects on the vasculature in general as well as on all stages of diabetic retinopathy, independent of its beneficial metabolic effects [8, 9]. The strength of these effects must be purposefully analysed in individuals with diabetes to determine the extent of linagliptin’s additional benefit in treating diabetes and preventing diabetic complications.
Data availability
All data generated or analysed during this study are included in this published article (and its ESM).
Abbreviations
- DPP-4:
-
Dipeptidyl peptidase 4
- ERK:
-
Extracellular signal-regulated kinase
- GLP:
-
Glucagon-like peptide
- GLP-1R:
-
Glucagon-like peptide 1 receptor
- HIF1A:
-
Hypoxia-inducible factor 1α
- HMGB-1:
-
High-mobility group box 1
- HUVEC:
-
Human umbilical vascular endothelial cell
- JNK:
-
c-Jun N-terminal kinase
- MAPK:
-
Mitogen-activated protein kinase
- NRP1:
-
Neuropilin 1
- OIR:
-
Oxygen-induced retinopathy
- PI3K:
-
Phosphoinositide 3-kinase
- qPCR:
-
Quantitative PCR
- SDF-1α:
-
Stromal cell-derived factor 1 α
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
References
Trikkalinou A, Papazafiropoulou AK, Melidonis A (2017) Type 2 diabetes and quality of life. World J Diabetes 8:120–129
Hammes H-P (2018) Diabetic retinopathy: hyperglycaemia, oxidative stress and beyond. Diabetologia 61:29–38
Gariano RF, Gardner TW (2005) Retinal angiogenesis in development and disease. Nature 438:960–966
Carmeliet P, Dor Y, Herbert JM et al (1998) Role of HIF-1α in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature 394:485–490
Duh EJ, Sun JK, Stitt AW (2017) Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight. https://doi.org/10.1172/jci.insight.93751
Mohamed Q, Gillies MC, Wong TY (2007) Management of diabetic retinopathy: a systematic review. JAMA 298:902–916
Darsalia V, Larsson M, Nathanson D et al (2015) Glucagon-like receptor 1 agonists and DPP-4 inhibitors: potential therapies for the treatment of stroke. J Cereb Blood Flow Metab 35:718–723
Drucker DJ, Nauck MA (2006) The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368:1696–1705
Salim HM, Fukuda D, Higashikuni Y et al (2016) Dipeptidyl peptidase-4 inhibitor, linagliptin, ameliorates endothelial dysfunction and atherogenesis in normoglycemic apolipoprotein-E deficient mice. Vasc Pharmacol 79:16–23
Dietrich N, Kolibabka M, Busch S et al (2016) The DPP4 inhibitor linagliptin protects from experimental diabetic retinopathy. PLoS One 11:e0167853
Lee C-S, Kim YG, Cho H-J et al (2016) Dipeptidyl peptidase-4 inhibitor increases vascular leakage in retina through VE-cadherin phosphorylation. Sci Rep 6:29393
Ajami K, Pitman MR, Wilson CH et al (2008) Stromal cell-derived factors 1α and 1β, inflammatory protein-10 and interferon-inducible T cell chemo-attractant are novel substrates of dipeptidyl peptidase 8. FEBS Lett 582:819–825
Odent Grigorescu G, Rosca A-M, Preda MB et al (2017) Synergic effects of VEGF-A and SDF-1 on the angiogenic properties of endothelial progenitor cells. J Tissue Eng Regen Med 11:3241–3252
Lima e Silva R, Shen J, Hackett SF et al (2007) The SDF-1/CXCR4 ligand/receptor pair is an important contributor to several types of ocular neovascularization. FASEB J 21:3219–3230
Song Z-Y, Wang F, Cui S-X, Qu X-J (2018) Knockdown of CXCR4 inhibits CXCL12-induced angiogenesis in HUVECs through downregulation of the MAPK/ERK and PI3K/AKT and the Wnt/β-catenin pathways. Cancer Investig 36:10–18
Butler JM, Guthrie SM, Koc M et al (2005) SDF-1 is both necessary and sufficient to promote proliferative retinopathy. J Clin Invest 115:86–93
Huan Y, Jiang Q, Liu J, Shen Z (2015) Establishment of a dipeptidyl peptidases (DPP) 8/9 expressing cell model for evaluating the selectivity of DPP4 inhibitors. J Pharmacol Toxicol Methods 71:8–12
Busek P, Stremenova J, Sedo A (2008) Dipeptidyl peptidase-IV enzymatic activity bearing molecules in human brain tumors—good or evil? Front Biosci 13:2319–2326
Thomas L, Eckhardt M, Langkopf E et al (2008) (R)-8-(3-amino-piperidin-1-yl)-7-but-2-ynyl-3-methyl-1-(4-methyl-quinazolin-2-ylmethyl)-3,7-dihydro-purine-2,6-dione (BI 1356), a novel xanthine-based dipeptidyl peptidase 4 inhibitor, has a superior potency and longer duration of action compared with other dipeptidyl peptidase-4 inhibitors. J Pharmacol Exp Ther 325:175–182
Scrocchi LA, Brown TJ, MaClusky N et al (1996) Glucose intolerance but normal satiety in mice with a null mutation in the glucagon-like peptide 1 receptor gene. Nat Med 2:1254–1258
Smith LE, Wesolowski E, McLellan A et al (1994) Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci 35:101–111
Abràmoff MD, Magalhaels P, Ram S (2004) Image processing with ImageJ. Biophoton Int 11:36–42
Selvam S, Kumar T, Fruttiger M (2017) Retinal vasculature development in health and disease. Prog Retin Eye Res 63:1–19
Parast CV, Mroczkowski B, Pinko C et al (1998) Characterization and kinetic mechanism of catalytic domain of human vascular endothelial growth factor receptor-2 tyrosine kinase (VEGFR2 TK), a key enzyme in angiogenesis. Biochemistry 37:16788–16801
Ozaki H, Yu AY, Della N et al (1999) Hypoxia inducible factor-1alpha is increased in ischemic retina: temporal and spatial correlation with VEGF expression. Invest Ophthalmol Vis Sci 40:182–189
Mazure NM, Chen EY, Laderoute KR, Giaccia AJ (1997) Induction of vascular endothelial growth factor by hypoxia is modulated by a phosphatidylinositol 3-kinase/Akt signaling pathway in Ha-ras-transformed cells through a hypoxia inducible factor-1 transcriptional element. Blood 90:3322–3331
Olsson A-K, Dimberg A, Kreuger J, Claesson-Welsh L (2006) VEGF receptor signalling—in control of vascular function. Nat Rev Mol Cell Biol 7:359–371
Ilan N, Mahooti S, Madri JA (1998) Distinct signal transduction pathways are utilized during the tube formation and survival phases of in vitro angiogenesis. J Cell Sci 111:3621–3631
Shibuya M (2013) VEGFR and type-V RTK activation and signaling. Cold Spring Harb Perspect Biol 5:a009092
Graupera M, Potente M (2013) Regulation of angiogenesis by PI3K signaling networks. Exp Cell Res 319:1348–1355
Wang XW, Zhang FX, Yang F et al (2016) Effects of linagliptin and liraglutide on glucose- and angiotensin II-induced collagen formation and cytoskeleton degradation in cardiac fibroblasts in vitro. Acta Pharmacol Sin 37:1349–1358
Liu N, Sun Y, Zhao N, Chen L (2014) Role of hypoxia-inducible factor-1α and survivin in oxygen-induced retinopathy in mice. Int J Clin Exp Pathol 7:6814–6819
Zhuge F, Ni Y, Nagashimada M et al (2016) DPP-4 inhibition by linagliptin attenuates obesity-related inflammation and insulin resistance by regulating M1/M2 macrophage polarization. Diabetes 65:2966–2979
Palodetto B, da Silva Santos Duarte A, Rodrigues Lopes M et al (2017) SEMA3A partially reverses VEGF effects through binding to neuropilin-1. Stem Cell Res 22:70–78
Cerani A, Tetreault N, Menard C et al (2013) Neuron-derived semaphorin 3A is an early inducer of vascular permeability in diabetic retinopathy via neuropilin-1. Cell Metab 18:505–518
Rivera JC, Sitaras N, Noueihed B et al (2013) Microglia and interleukin-1β in ischemic retinopathy elicit microvascular degeneration through neuronal semaphorin-3A. Arterioscler Thromb Vasc Biol 33:1881–1891
Hebsgaard JB, Pyke C, Yildirim E et al (2018) Glucagon-like peptide-1 receptor expression in the human eye. Diabetes Obes Metab. https://doi.org/10.1111/dom.13339
Remm F, Kränkel N, Lener D et al (2018) Sitagliptin accelerates endothelial regeneration after vascular injury independent from GLP1 receptor signaling. Stem Cells Int 2018:5284963
Wang X, Ding Z, Yang F et al (2016) Modulation of myocardial injury and collagen deposition following ischaemia-reperfusion by linagliptin and liraglutide, and both together. Clin Sci (Lond) 130:1353–1362
Hammes H-P, Feng Y, Pfister F, Brownlee M (2011) Diabetic retinopathy: targeting vasoregression. Diabetes 60:9–16
Funding
This study was funded and supported by Boehringer Ingelheim. MK is an associated member of the GRK1874 DIAMICOM, funded by the Deutsche Forschungsgemeinschaft.
Author information
Authors and Affiliations
Contributions
MK, ND and HPH contributed to the conception and design of this study, acquisition, analysis and interpretation of data, reviewed the literature and critically drafted and revised the manuscript. TK contributed to acquisition, analysis and interpretation of data, reviewed the literature and critically drafted and revised the manuscript. All authors approved the final version of the manuscript. MK and HPH are responsible for the integrity of the work as a whole.
Corresponding authors
Ethics declarations
All authors declare that there is no duality of interest associated with this manuscript. TK is a full-time employee of Boehringer Ingelheim. Boehringer Ingelheim had no influence on the conception and design of this study, or on the decision to publish the results.
Electronic supplementary material
ESM
(PDF 139 kb)
Rights and permissions
About this article
Cite this article
Kolibabka, M., Dietrich, N., Klein, T. et al. Anti-angiogenic effects of the DPP-4 inhibitor linagliptin via inhibition of VEGFR signalling in the mouse model of oxygen-induced retinopathy. Diabetologia 61, 2412–2421 (2018). https://doi.org/10.1007/s00125-018-4701-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4701-4