Abstract
Purpose
Bereavement research has helped to improve end-of-life practices in the ICU. However, few studies have explored bereaved relatives experience of research participation in this context. We aimed to explore the experience of bereaved relatives’ participation in the ARREVE study which included three telephone follow-up calls to complete several quantitative tools.
Methods
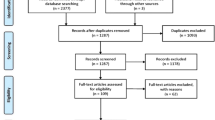
Volunteer relatives who participated in the 12-month follow-up call completed a questionnaire about research participation that included ten open-ended questions so that respondents could use their own words and thoughts. These open-ended questions were analyzed using qualitative analysis that examines themes within the data.
Results
175/311 relatives completed the questionnaire. Three themes were derived from the thematic analysis: (1) struggling: reactivation of emotional distress associated with the ICU experience and the loss is frequent, specifically during the 1st follow-up call. (2) Resilience: as time goes by, research participation becomes increasingly positive. The calls are a help both in giving meaning to the relatives’ experience and in accepting the loss. (3) Recognition: research calls can compensate for the absence of support during bereavement.
Conclusion
Although some emotional difficulties must be acknowledged, bereavement research is overall associated with benefits, by facilitating emotional adjustments, meaning-making and resilience. Lack of support and social isolation during bereavement are frequent experiences, revealing that support strategies for bereaved relatives should be developed after the loss of a loved one in the ICU.

Similar content being viewed by others
References
Lautrette A, Darmon M, Megarbane B et al (2007) A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 356(5):469–478
Kentish-Barnes N, Chaize M, Seegers V et al (2015) Complicated grief after death of a loved one in the intensive care unit. Eur Respir J 45:1341–1352
Carson SS, Cox CE, Wallenstein S et al (2016) Effect of palliative care-led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA 316(1):51–62
Curtis JR, Treece PD, Nielsen EL et al (2016) Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. Am J Respir Crit Care Med 193(2):154–162
Kentish-Barnes N, Chevret S, Champigneulle B et al (2017) Effect of a condolence letter on grief symptoms among relatives of patients who died in the ICU: a randomized clinical trial. Intensive Care Med 43(4):473–484
Butler AE, Hall H, Copnell B (2018) Bereaved parents’ experiences of research participation. BMC Palliat Care 17:122–130
Dyregrov K (2004) Bereaved parents’ experience of research participation. Soc Sci Med 58:391–400
Hynson J, Aroni R, Bauld C, Sawyer S (2006) Research with bereaved parents: a question of how and not why. Palliat Med 20(8):805–811
Kentish-Barnes N, Chevret S, Cheisson G et al (2018) Grief symptoms in relatives who experienced organ donation requests in the ICU. Am J Respir Crit Care Med 198(6):751–758
Kentish-Barnes N, McAdam JL, Kouki S et al (2015) Research participation for bereaved family members: experience and insights from a qualitative study. Crit Care Med 43(9):1839–1845
Kubler-Ross E (1969) On death and dying. The Macmillan Company, New York
Robert R, Le Gouge A, Kentish-Barnes N et al (2017) Terminal weaning or immediate extubation for withdrawing mechanical ventilation in critically ill patients (the ARREVE observational study). Intensive Care Med 43(12):1793–1807
McAdam JL, Arai S, Puntillo KA (2008) Unrecognized contributions of families in the intensive care unit. Intensive Care Med 34:1097–1101
Bazeley P, Jackson K (2013) Qualitative data analysis with Nvivo, 2nd edn. SAGE Publications Ltd, London
Cook AS, Bosley G (1995) The experience of participating in bereavement research: stressful or therapeutic? Death Stud 19(2):157–170
Stroebe M, Stroebe W, Schut H (2003) Bereavement research: methodological issues and ethical concerns. Palliat Med 17(3):235–240
Rosenblatt PC (1995) Ethics of qualitative interviewing with grieving families. Death Stud 19(2):139–155
Parkes CM (1995) Guidelines for conducting ethical bereavement research. Death Stud 19(2):171–181
Luthar SS, Cicchetti D, Becker B (2000) The construct of resilience: a critical evaluation and guidelines for future work. Child Dev 71(3):543–562
Fonagy P, Steele M, Steele H et al (1994) The theory and practice of resilience. J Child Psychol Psychiatry 35:231–257
Barnato AE, Schenker Y, Tiver G et al (2017) Storytelling in the early bereavement period to reduce emotional distress among surrogates involved in a decision to limit life support in the ICU: a pilot feasibility trial. Crit Care Med 45(1):35–46
Meert KL, Eggly S, Kavanaugh K et al (2015) Meaning making during parent-physician bereavement meetings after a child’s death. Health Psychol 34(4):453–461
Nelson JE, Puntillo KA, Pronovost PJ et al (2010) In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med 38(3):808–818
Stroebe M, Boerner K (2015) Caregiving and bereavement research: bridges over the gap. Palliat Med 29(7):574–576
Haines KJ, Sevin CM, Hibbert E et al (2019) Key mechanisms by which post-ICU activities can improve in-ICU care: results of the international THRIVE collaboratives. Intensive Care Med 45:939–947
Cunningham TV, Scheunemann LP, Arnold RM, White D (2018) How do clinicians prepare family members for the role of surrogate decision-maker? J Med Ethics 44(1):21–26
Acknowledgements
Vanessa Zinzoni (research nurse), Isabelle Treillet (psychologist), Cedric Colombo (psychologist).
Funding
The ARREVE study was supported by grants from three non-profit organizations: the Fondation de France (#000332577), La Roche-sur-Yon Departmental Hospital, and Programme Hospitalier de Recherche Clinique National 2012 of the French Ministry of Health (#13-0142).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alexandra Laurent, Jean Reignier, Amélie Le Gouge, Elie Azoulay, René Robert and Nancy Kentish-Barnes designed the study, analyzed the data and wrote the original manuscript. Alice Cottereau, Mélanie Adda, Djillali Annane, Juliette Audibert,François Barbier, Patrick Bardou, Simon Bourcier, Jeremy Bourenne, Alexandre Boyer, François Brenas, Vincent Das, Arnaud Desachy, Jérôme Devaquet, Marc Feissel, Frédérique Ganster, Maïté Garrouste-Orgeas, Guillaume Grillet, Olivier Guisset, Rebecca Hamidfar-Roy, Anne-Claire Hyacinthe, Sebastien Jochmans, Mercé Jourdain, Alexandre Lautrette, Nicolas Lerolle, Olivier Lesieur, Fabien Lion, Philippe Mateu, Bruno Megarbane, Sybille Merceron, Emmanuelle Mercier, Jonathan Messika, Paul Morin-Longuet, Bénédicte Philippon-Jouve, Jean-Pierre Quenot, Anne Renault, Xavier Repesse, Jean-Philippe Rigaud, Ségolène Robin, Antoine Roquilly, Amélie Seguin, Didier Thevenin, Patrice Tirot, Isabelle Vinatier participated in meetings held to improve the original design and organization of the ARREVE studies, participated in acquiring the data and writing the manuscript. All authors approved the final version of the manuscript and have agreed to be accountable for the work it reports.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Laurent, A., Reignier, J., Le Gouge, A. et al. “You helped me keep my head above water”—experience of bereavement research after loss of a loved one in the ICU: insights from the ARREVE study. Intensive Care Med 45, 1252–1261 (2019). https://doi.org/10.1007/s00134-019-05722-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05722-x