Abstract
Introduction and hypothesis
Our aim was to calculate the total radiation exposure and the dose absorbed by specific organs during videourodynamics (VUDS) in women.
Methods
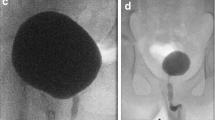
This was a retrospective study of consecutive women attending for VUDS in a tertiary referral urodynamics unit. Tests with missing data and those that were terminated during the filling phase of the cystometry were excluded from the study. The VUDS examination was tailored according to the indication for the test and the urodynamic question to be answered. The PCXMC simulation program (version 2.0) was utilised to calculate the effective dose and the dose absorbed by individual organs.
Results
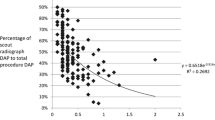
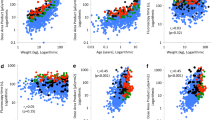
Out of 345 consecutive VUDS, 264 were included in the study. The mean effective dose was 0.34 mSv (SD: 0.15) and the mean fluoroscopic time was 63.15 s (SD: 21.81). Multivariate linear regression analysis of factors affecting the radiation dose showed that BMI (p = 0.009) and fluoroscopy time (p < 0.001) were the only statistically significant factors. The final linear regression model for the estimation of the effective dose was Eff. Dose (mSv) = −0.049 + 0.003 · BMI (kg/m2) + 0.005 · fluoroscopy time (s).
Conclusions
This study reveals that women are exposed to relatively small amounts of radiation during VUDS. The use of fluoroscopy only without additional static radiographic images minimises exposure to a level consistent with the “as low as reasonably achievable” radiological principle.
Similar content being viewed by others
References
Bates CP, Whiteside CG, Turner-Warwick R (1970) Synchronous cine-press-flow-cysto-urethrography with special reference to stress and urge incontinence. Br J Urol 42:714–723
Abrams P (2006) Urodynamics, 3rd edn. Springer, London, pp 88–94
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Nitti VW, Tu LM, Gitlin J (1999) Diagnosing bladder outlet obstruction in women. J Urol 161:1535–1540
Tubaro A, Artibani W, Bartram C, Delancey J, Khullar V, Vierhout M et al (2009) Imaging and other investigations. In: Abrams P, Cardozo L, Khoury S, Wein A (eds) Incontinence, 4th International Consultation on Incontinence, 4th edn. Health Publications Ltd, Paris, pp 541–630
Hart D, Wall BF, Hillier MC, Shrimpton PC (2010) Frequency and collective dose for medical and dental X-ray examinations in the UK, 2008. Report HPA –CRCE-012. www.hpa.org.uk
Arbique GM, Gilleran JP, Guild JB, Harris JE, Poon CI, Zimmern PE (2006) Radiation exposure during standing voiding cystourethrography in women. Urology 67:269–274
International Commission on Radiological Protection (2007) Recommendations of the International Commission on Radiological Protection. Publication 103. Ann ICRP 37:2–4
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Schafer W, Abrams P, Liao L et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry and pressure-flow studies. Neurourol Urodyn 21:261–274
Servomaa A, Tapiovvara M (1998) Organ dose calculation in medical x ray examinations by the program PCXMC. Radiat Prot Dosim 80:213–219
International Commission on Radiological Protection (1991) Recommendations of the International Commission on Radiological Protection. Publication 60. Ann ICRP 21:1–3
Darling S, Sammer M, Chapman T, Parisi MT (2011) Physician documentation of fluoroscopy in voiding cystourethrography reports correlates with lower fluoroscopy times: a surrogate marker of patient radiation exposure. AJR Am J Roentgenol 196:W777–W780
Guild J, Takacs E, Kircher S, Arbique G, Zimmern PE (2009) The number of voiding radiographs during cystourethrography in women with stress incontinence or prolapse can be reduced to enhance safety without compromising study interpretation. Neurourol Urodyn 28:385–389
Lee CL, Wunderle K, Vasavada SP, Goldman HB (2011) Reduction of radiation during fluoroscopic urodynamics: analysis of quality assurance protocol limiting fluoroscopic images during fluoroscopic urodynamic studies. Urology 78:540–543
Singh G, Lucas M, Dolan L, Knight S, Ramage C, Toozs-Hobson P (2010) Minimum standards for urodynamic practice in the UK. Neurourol Urodyn 29:1365–1372
Perisinakis K, Damilakis J, Grammatikakis J, Theocharopulos N, Gourtsoyiannis N (2003) Radiogenic risks from hysterosalpingography. Eur Radiol 13:1522–1528
Lee R, Thomas KE, Connolly BL, Falkiner M, Gordon CL (2009) Effective dose estimation for pediatric voiding cystourethrography using an anthrophomorphic phantom set and metal oxide semiconductor field-effect transistor (MOSFET) technology. Pediatr Radiol 39:608–615
Hart D, Hillier MC, Wall BF (2007) Doses to patients from radiographic and fluoroscopic X-ray imaging procedures in the UK, 2005. Report HPA –RPD-029. www.hpa.org.uk
Conflicts of interest
I Giarenis—none
J Phillips—none
H Mastoroudes—none
S Srikrishna—speaker honorarium: Astellas
D Robinson—consultant: Astellas, Ferring, Gynaecare, Pfizer; speaker honorarium: Astellas, Ferring, Gynaecare, Pfizer; trial participation: Astellas, Pfizer
C Lewis—none
L Cardozo—consultant: Allergan, Astellas, Merck, Pfizer, Teva; speaker honorarium: Astellas, Merck, Pfizer; trial participation: Astellas, Pfizer
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giarenis, I., Phillips, J., Mastoroudes, H. et al. Radiation exposure during videourodynamics in women. Int Urogynecol J 24, 1547–1551 (2013). https://doi.org/10.1007/s00192-013-2062-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2062-6