Abstract
Purpose
To investigate the novel zein-based non-adhesive precipitating liquid embolic HEIE1_2017.
Materials and Methods
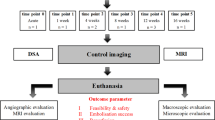
Zein-based liquid embolics are an own class of embolization material. In this study, HEIE1_2017, a novel zein-based liquid embolic, was investigated. Visibility was assessed in vitro in CT and MRI phantoms, embolization characteristics were assessed in vivo in the kidneys of 12 pigs. Components of HEIE1_2017 were zein as occlusion material, ethanol as solvent, and iodized oil as radiopaque material. HEIE1_2017 was used in pure (HEI-PURE) and manually modified (HEI-MOD) form and compared with 6% ethylene vinyl alcohol copolymer (EVOH). Different radiological methods (CT, MRI, DSA, cone-beam CT, and micro-CT) and histopathologic analyses were applied to compare visibility and vascular occlusion patterns.
Results
In CT phantoms, all embolics were definitely visible as hyperdense materials. In MRI phantoms, signal-to-noise ratio was highest for HEI-PURE, followed by HEI-MOD and EVOH. In all kidneys, embolization procedures were technically successful and without complications. In DSA, all embolics were definitely visible during and after embolization. Only EVOH caused substantial artifacts in cone-beam CT and CT. In micro-CT and histopathology, HEI-PURE showed a homogeneous occlusion from segmental arteries to glomerular capillaries. HEI-MOD demonstrated the deepest vascular penetration (up to the level of peritubular capillaries), but with an inhomogeneous distribution. For EVOH, there was inhomogeneous vascular occlusion from segmental arteries to glomerular capillaries.
Conclusion
HEIE1_2017 is a promising novel zein-based liquid embolic. Further preclinical and clinical studies with higher case numbers and long-term follow-up are needed to further assess the value of this embolic material.






Similar content being viewed by others
References
Akmangit I, Daglioglu E, Kaya T, et al. Preliminary experience with squid: a new liquid embolizing agent for AVM, AV fistulas and tumors. Turk Neurosurg. 2014;24(4):565–70.
Bartling SH, Budjan J, Aviv H, et al. First multimodal embolization particles visible on X-ray/computed tomography and magnetic resonance imaging. Investig Radiol. 2011;46(3):178–86.
Bisdorff A, Mazighi M, Saint-Maurice JP, Chapot R, Lukaszewicz AC, Houdart E. Ethanol threshold doses for systemic complications during sclerotherapy of superficial venous malformations: a retrospective study. Neuroradiology. 2011;53(11):891–4.
Brown PA, Zomorodi AR, Gonzalez LF. Endovascular management of spinal dural arteriovenous fistulas. Handb Clin Neurol. 2017;143:199–213.
Buecker A, Keulers P, Guenther RW. Successful closure and embolization of a fistula between the pancreatic duct and a pseudocyst using ethibloc. Cardiovasc Interv Radiol. 1997;20(5):394–6.
De Beule T, Vranckx J, Verhamme P, et al. Transarterial embolization of peripheral arteriovenous malformations with ethylenevinyl alcohol copolymer: feasibility, technical outcomes, and clinical outcomes. Vasa. 2016;45(6):497–504.
Desir A, Ghaye B, Duysinx B, Dondelinger RF. Percutaneous sclerotherapy of a giant mediastinal lymphangioma. Eur Respir J. 2008;32(3):804–6.
Doerfler A, Goericke S, Wanke I, Holla M, Forsting M. Flow-directed microcatheters for cerebral embolizations using Ethibloc: an in vitro study. Neuroradiology. 2001;43(12):1112–7.
Elsenousi A, Aletich VA, Alaraj A. Neurological outcomes and cure rates of embolization of brain arteriovenous malformations with n-butyl cyanoacrylate or Onyx: a meta-analysis. J Neurointerv Surg. 2016;8(3):265–72.
Eom HJ, Shin JH, Cho YJ, Nam DH, Ko GY, Yoon HK. Transarterial embolisation of renal arteriovenous malformation: safety and efficacy in 24 patients with follow-up. Clin Radiol. 2015;70(11):1177–84.
George HL, Unnikrishnan PN, Garg NK, Sampath JS, Bass A, Bruce CE. Long-term follow-up of Ethibloc injection in aneurysmal bone cysts. J Pediatr Orthop B. 2009;18(6):375–80.
Gross BA, Albuquerque FC, Moon K, McDougall CG. Evolution of treatment and a detailed analysis of occlusion, recurrence, and clinical outcomes in an endovascular library of 260 dural arteriovenous fistulas. J Neurosurg. 2017;126(6):1884–93.
Gross BA, Moon K, McDougall CG. Endovascular management of arteriovenous malformations. Handb Clin Neurol. 2017;143:59–68.
Hansmann HJ, Hallscheidt P, Aretz K, Kauffmann GW, Richter GM. Renal tumor embolization. Radiologe. 1999;39(9):783–9.
Kauffmann GW, Richter GM, Rohrbach R, Wenz W. Prolonged survival following palliative renal tumor embolization by capillary occlusion. Cardiovasc Interv Radiol. 1989;12(1):22–8.
Khaja MS, Park AW, Swee W, et al. Treatment of type II endoleak using Onyx with long-term imaging follow-up. Cardiovasc Interv Radiol. 2014;37(3):613–22.
Klauss M, Heye T, Stampfl U, Grenacher L, Radeleff B. Successful arterial embolization of a giant pseudoaneurysm of the gastroduodenal artery secondary to chronic pancreatitis with literature review. J Radiol Case Rep. 2012;6(2):9–16.
Konya A, Wright KC. Capillary embolization using ethiodol-ethanol for complete renal ablation in Swine. Investig Radiol. 2002;37(9):512–20.
Kramer SC, Gorich J, Rilinger N, et al. Embolization for gastrointestinal hemorrhages. Eur Radiol. 2000;10(5):802–5.
Lubicz B, Piotin M, Mounayer C, Spelle L, Moret J. Selective endovascular treatment of intracranial aneurysms with a liquid embolic: a single-center experience in 39 patients with 41 aneurysms. AJNR Am J Neuroradiol. 2005;26(4):885–93.
Mironov A. Embolization of meningiomas using liquid embolizing agents. Rofo. 1990;153(3):327–34.
Poursaid A, Jensen MM, Huo E, Ghandehari H. Polymeric materials for embolic and chemoembolic applications. J Control Release. 2016;240:414–33.
Radeleff B, Schawo S, Hoffmann K, et al. Efficacy and safety of percutaneous transhepatic portal embolization before right liver resection using an ethibloc/lipiodol mixture: a single-center experience. Dig Surg. 2008;25(1):52–9.
Rangel-Castilla L, Shah AH, Klucznik RP, Diaz OM. Preoperative Onyx embolization of hypervascular head, neck, and spinal tumors: experience with 100 consecutive cases from a single tertiary center. J Neurointerv Surg. 2014;6(1):51–6.
Rassweiler J, Prager P, Haferkamp A, Alken P, Kauffmann GW, Richter G. Transarterial nephrectomy: the current status of experimental and clinical studies. J Endourol. 2008;22(4):767–82.
Richter G, Rassweiler J, Kauffmann GW, Wenz W, Crawford DB. Experimental study of the effectiveness of capillary embolization using contrast-enhanced Ethibloc. Invest Radiol. 1984;19(1):36–44.
Roberts DA, Balter JM, Chaudhary N, Gemmete JJ, Pandey AS. Dosimetric measurements of Onyx embolization material for stereotactic radiosurgery. Med Phys. 2012;39(11):6672–81.
Sadeh-Gonike U, Magand N, Armoiry X, et al. Transarterial Onyx embolization of intracranial dural fistulas: a prospective cohort, systematic review, and meta-analysis. Neurosurgery. 2018;82(6):854–63.
Saeed Kilani M, Izaaryene J, Cohen F, et al. Ethylene vinyl alcohol copolymer (Onyx(R)) in peripheral interventional radiology: indications, advantages and limitations. Diagn Interv Imaging. 2015;96(4):319–26.
Sommer CM, Stampfl U, Bellemann N, et al. Patients with life-threatening arterial renal hemorrhage: CT angiography and catheter angiography with subsequent superselective embolization. Cardiovasc Interv Radiol. 2010;33(3):498–508.
Vollherbst DF, Otto R, Do T, et al. Imaging artifacts of Onyx and PHIL on conventional CT, cone-beam CT and MRI in an animal model. Interv Neuroradiol. 2018;24:693–701.
Vollherbst DF, Otto R, von Deimling A, et al. Evaluation of a novel liquid embolic agent (precipitating hydrophobic injectable liquid (PHIL)) in an animal endovascular embolization model. J Neurointerv Surg. 2018;10(3):268–74.
Vollherbst DF, Sommer CM, Ulfert C, Pfaff J, Bendszus M, Mohlenbruch MA. Liquid embolic agents for endovascular embolization: evaluation of an established (Onyx) and a novel (PHIL) embolic agent in an in vitro AVM model. AJNR Am J Neuroradiol. 2017;38(7):1377–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vollherbst, D.F., Do, T.D., Jugold, M. et al. The Novel X-Ray Visible Zein-Based Non-adhesive Precipitating Liquid Embolic HEIE1_2017: An Exploratory Study. Cardiovasc Intervent Radiol 42, 905–914 (2019). https://doi.org/10.1007/s00270-019-02179-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-019-02179-9