Abstract
Among emerging and re-emerging infectious diseases, influenza constitutes one of the major threats to mankind. In this review series epidemiologic, virologic and pathologic concerns raised by infections of humans with avian influenza virus A/H5N1 are discussed. This fourth part focuses on vaccine development. Several phase I clinical studies with vaccines against H5 viruses have demonstrated limited efficacy compared to seasonal influenza vaccines. To induce protective immunity two immunisations with increased amounts of H5N1 vaccine were required. Novel vaccination strategies that are egg- and adjuvant-independent, broadly cross-reactive and long-lasting are highly desirable.
Similar content being viewed by others
Introduction
Highly pathogenic avian influenza (H5N1 strain) continues to cause outbreaks in poultry and migratory birds in Asia, Europe, and Africa. Recently, humans became infected by this virus with both increasing number of infected individuals and high mortality rates [1–3] suggesting persisting threat of human H5N1 pandemic. Antiviral drugs such as neuraminidase inhibitors are valuable for the prevention and treatment of H5N1 infections, however, they are limited in supply and resistance to these antivirals has been described in multiple isolates [4–6]. Therefore, development of an H5N1 vaccine is recognised as the primary strategy to protect humans against a possible H5N1 pandemic. Currently, 16 manufacturers from 10 countries are known to develop prototype human pandemic vaccines against H5N1 influenza.
Genomic and antigenic analysis of H5N1 viruses isolated since 2004 revealed at least two distinct sublineages with different geographic distributions designated clade 1 and 2 [1, 7]. Clade 2 viruses are specified as subclades 1, 2 and 3, whereas for clade 1 there are currently no subclades. Human infections were caused mainly by H5N1 viruses from clade 1 in 2004–2005 in Cambodia, Thailand and Vietnam. In contrast, since later 2005 most human infections have been due clade 2 viruses, primarily subclade 1 in Indonesia, subclade 2 in countries in the Middle East, Europe, and Africa, and subclade 3 in China. Reports of genetic and antigenic changes observed in the H5N1 virus isolates have raised concern about the ability of a vaccine generated from a single selected strain to protect against a diverse set of viruses. Therefore, major focus in H5N1 vaccine development is on testing of vaccine candidates for priming, cross-reactivity and cross-protection against infection with viruses from different clades and subclades.
Principles that have been established for the research of human influenza in general are also applicable to pandemic H5N1 influenza vaccine development. However, several practical and scientific challenges, specific for the development of H5N1 vaccines exist [8–10]. These include high pathogenicity of wild-type H5N1 influenza viruses, poor immunogenicity (for unknown reasons) of the H5 haemagglutinin (HA) as well as sparse information on the antigenic sites on avian HAs and the immune correlates of protections from avian influenza-infections. Reduced yield of candidate vaccine viruses in embryonic hen’s eggs compared to that of human-adapted influenza viruses and limited manufacturing capacity represent additional obstacles in development of H5N1 vaccine. Different approaches have been used to generate candidates for human H5N1 vaccine including those based on the use of licensed technology, such as inactivated or live attenuated vaccines. In the present review, we discuss several H5N1 vaccines of these types which are under development, as well as some that do not fall into either category, where a degree of genetic manipulation is involved (Tables 1, 2).
Protective immunity against influenza
A development of effective vaccine depends on understanding of protective immune responses against natural infection, particularly those directed against specific virus constituents (Table 3). The influenza virus major surface glycoproteins HA and neuraminidase (NA) are the principal targets of the protective immune response [11, 12]. HA specific antibodies neutralise the infectivity of the virus and prevent infection by antigenically related influenza viruses. In contrast, NA specific antibodies do not prevent influenza virus infection but prevent the release of viruses from infected cells, and NA immunity is referred to as infection permissive [13]. Antibodies to the matrix M2 protein, which is conserved within the A-type influenza viruses, are cross-protective between different subtype-virus infections, although the level of protection is low [14]. Antibodies to the conserved nucleoprotein (NP) and matrix M1 protein can be induced, although they fail to contribute to protection. This was demonstrated by failure of passive transfer of M1 or NP monoclonal antibodies in mice to protect from challenge by a wild-type influenza virus [15]. Peptides generated from influenza endogenous antigens, synthesised within the infected cells, are targets for cytotoxic lymphocytes (CTLs), which destroy infected cells presenting the peptide- major histocompability class I (MHC class I) complexes [16, 17]. Among the endogenous antigens, internal antigens are major targets for CTLs. NP is the strongest of these antigens [18, 19]. However, human CTL responses to influenza A virus may be also directed against surface glycoproteins HA and NA, matrix proteins M1 and M2 and non-structural protein 1 (NS1) [20]. CTLs show cross-reactivity in their recognition of the different subtypes of human influenza A virus [16, 20]. Recently, conserved CTL epitopes were detected in internal proteins of different isolates of the highly pathogenic H5N1 influenza virus [19]. These findings demonstrate that HA specific antibodies are primarily responsible for preventing infection, while NA specific antibodies and CTLs specific for different viral proteins are responsible for reducing viral spread and thereby for accelerating the recovery from influenza.
Antibodies directed at the HA and NA surface glycoproteins of the virus are effective in mediating protection that is long-lived in the absence of antigenic drift (i.e., mutations in and around the antibody-recognition sites of the HA and NA) or shift (i.e., introduction of a novel HA and/or NA) in circulating viruses. A role for the protection through homotypic antibodies was evident in 1977 when an H1N1 virus that had circulated in the early 1950s reappeared in the human population [21, 22]. Significant disease was only seen in persons born after the H1N1 virus had stopped circulating in 1957, indicating that homotypic immunity is long-lived. On the other hand, the epidemiologic behaviour of influenza viruses in humans suggests that infection with one subtype induces little or no immunity to other subtypes [12, 15, 23]. The overall contribution of CTLs to providing heterosubtypic protection and disease reduction during reinfection with the influenza A is small. This has been recognised in individuals born after 1957 who were infected multiple times with H2N2 or H3N2 viruses before infection with H1N1 virus despite these different virus types share internal protein antigens which are targets for CTLs. Similarly, the contribution of cross-reactive antibodies to providing heterosubtypic cross-protection in humans may be small, particularly in children. Analysis of epidemiological data collected before and during the 1957 pandemic (during which a shift from subtype H1N1 to H2N2 occurred) suggests that heterosubtypic immunity occurred in adults but not in children [24]. However, these historical data alone cannot prove the existence of cross-protection in humans or establish its mechanisms.
The emergence in 1968 of an H3N2 influenza virus with a novel HA subtype (H3) provided an opportunity to evaluate a role of NA-specific antibodies in protection from influenza illness in humans. In a cohort of individuals with varying levels of N2 specific serum antibody, the severity of clinical illness correlated with the level of NA specific serum antibody present at the time of H3N2 virus challenge [25]. However, even when the NA was fully conserved between the previously circulating H2N2 virus and the newly emerged H3N2 virus, and NA immunity may have decreased the severity of the pandemic, it was not sufficient to prevent morbidity and mortality associated with the 1968 influenza pandemic [26]. Recently the NA immunity became a focus of attention as a possible protection against avian H5N1 infection. It has been demonstrated that vaccination of mice with DNA encoding NA from human H1N1 (A/Puerto Rico/8/34) induces sufficient humoral immunity to provide partial protection against H5N1 infection. The evidence was also provided that approximately 20% of the human population have anti-NA antibodies that crossreact at low titers with the N1 of avian H5N1 (A/Vietnam/1203/04) [27]. These data, however, are insufficient to conclude that humans with N1 NA humoral immunity will be protected against prospective avian influenza virus H5N1 infection. Nevertheless, the components of immune response, such as NA-specific protection or heterosubtypic immunity, should be further investigated as they may have implication for influenza vaccination.
Inactivated whole-virus vaccines
Inactivated whole-virus influenza vaccines provide virus particles, which are rendered harmless by inactivation with formaldehyde or β-propiolactone. Processing this way makes all of the antigens of the virus available to the immune system. Because of virus inability to replicate in vivo, inactivated vaccines (both whole and subvirion) are generally less immunogenic than live vaccines. To improve the immunogenecity of a conventional vaccine adjuvants such as aluminium hydroxide, aluminium phosphate, MF59 and new approaches such as virosome carrier/adjuvant system are being investigated [28]. The inclusions of adjuvants may reduce doses of vaccine antigen and this extend a limited vaccine supply in a pandemic situation. Aluminium salts when combined as an adjuvant with whole virus H2N2 and H9N2 vaccine allowed an eightfold reduction in antigen content while maintaining immunogenicity [29, 30]. However, in unprimed individuals two-dose schedule of the vaccine were required to achieve maximal mean antibody titre [29]. A significance of priming for vaccination was demonstrated in trials with an inactivated whole-virus H9N2 vaccine. It was immunogenic in individuals who had circulating antibodies induced by prior exposure to H2N2 viruses that cross-reacted with H9N2 viruses. However, the vaccine was not immunogenic in individuals who were born after 1968, when H2N2 stopped circulating in humans [9].
Inactivated vaccines do not effectively elicit cell-mediated immunity (particularly CTLs) because of general lack of access of exogenous vaccine-administered antigens to endogenous MHC class I antigen presentation pathway. In vitro experiments using human adapted seasonal influenza viruses revealed the following two conditions required for the presentation of a viral antigen by dendritic cells (DCs) to naïve CTLs: (1) influenza need to be infectious and (2) presentation of MHC class I-dependent influenza virus antigen utilises the endogenous pathway, but not the alternative cross-presentation pathway of antigen presentation [31–33]. The lack of cross-presentation of the influenza antigen was not caused by poor uptake of inactivated virus by DCs, because the incubation of DCs with inactivated virus did stimulate CD4+ T cell responses [31]. Stronger induction of CTL responses resulting from access of viral antigens to endogenous MHC class I presentation pathway was found in attenuated live vaccine, thus providing an advantage over inactivated vaccine. On the other hand, inactivated vaccines are particularly useful for presenting conformational antibody epitopes found on the surface of influenza viruses.
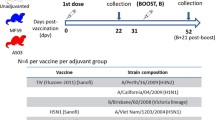
The conventional strategy for inactivated influenza vaccine (both whole and subvirion) uses seed virus, which must be antigenically similar to the circulating H5N1 viruses [22]. There are two basic approaches of how to prepare seed virus for a pandemic vaccine such as H5N1 influenza. First approach uses naturally occurring (not genetically modified) seed virus, which possess low pathogenicity and grows efficiently in eggs, an important characteristic for vaccine production. The second strategy involves the production of vaccine from modified viruses isolated from infected humans. In this approach candidate H5N1 strains are prepared by reverse genetics technology using attenuated viruses, the HA and NA of which were derived from a human H5N1 virus and the rest of their genes from an influenza A virus (known as backbone virus) that grows well in eggs (Fig. 1) [34–37]. For the H5N1 vaccine strains, the attenuation is achieved by modification of the cleavage-site sequence of the HA gene from virulent- to avirulent-type sequences without influencing antigenicity. World Health Organization (WHO) has approved the use of A/Puerto Rico/8/34 (H1N1-PR8) as a backbone virus. PR8, originally a human isolate, has been proven to be attenuated in humans and has previously grown well in eggs [35]. However, most manufacturers report that yields of antigen from reverse genetics-derived H5N1 viruses are lower than those of seasonal influenza viruses, reducing the quantity of antigen available for vaccine formulation [9]. There is an urgent need to improve the yield of reverse genetics-derived H5N1 viruses in eggs, which necessitates an improved understanding of the molecular basis of influenza replicative capacity. Several high-growth viruses (PR8-H5N1, 6:2 reassortant), including NIBRG-14 (produced by National Institute for Biological Standards and Control, UK), VN/04xPR8-rg (produced by St Jude Children’s Research Hospital, USA) and VNH5N1-PR8/CDC-rg (produced by Centers for Disease Control and Prevention, USA) have been developed by reverse genetics as potential seed viruses for inactivated vaccine [38, 39].
The eight-plasmid reverse genetics system. Full-length cDNA of high pathogenic (HP) avian virus HA, modified so that its cleavage-site coding sequences were altered from virulent to avirulent, and wild-type NA of H5N1 virus were cloned into plasmids with dual promoters that allow synthesis of both negative-sense viral RNA and positive sense mRNA. Full-length cDNAs of the other six internal gene segments were cloned into the same plasmid vector from the high-growth donor A/PR/8/34 (H1N1) virus. Cell line that is certified for vaccine strain preparation (e.g. Vero cells) is transfected with the plasmids, and the ressortant virus is isolated. The recombinant viruses may be used as inactivated whole-virion or split vaccine. Live attenuated vaccine may be prepared by modification of donor virus as shown here for a deletion of NS1 gene, the main antagonist of the IFN response of the host
A whole virus inactivated vaccine from reverse genetics-derived H5N1 influenza virus A/Vietnam/1194/04 and PR8 backbone virus with aluminium hydroxide-adjuvant was recently tested in China [40]. A stratified randomised, placebo-controlled, double-blind Phase I clinical trial was done in 120 volunteers aged 18–60. Antibody response was detected after two doses of 10 μg HA resulting in seropositivity in 78 and 96% of recipients by haemagglutinin inhibition and neutralization assay, respectively. A two-dose regimen met all European regulatory requirements for annual licensing of seasonal influenza vaccine. Similar results were reported from Hungary in a study of aluminium phosphate-adjuvanted whole-virus vaccine prepared from reverse genetics-derived influenza A/Vietnam/1194/04 and PR8 virus. A single dose, containing 6 μg antigen, induced seroconversions in 68% of 146 recipients [9]. Although whole-virion H5N1 vaccine was well tolerated [40], earlier whole-virion vaccines were associated with febrile reactions, particularly in children [41, 42]. Having in mind the potential disruption by pandemic influenza, modest reactogenicity might be acceptable. However, careful investigation is needed before widespread immunisation with this type of H5N1 vaccine.
The clinical studies described above have used whole-virus inactivated vaccines derived from clade 1 H5N1 viruses isolated in 2003 and 2004. It is not clear whether vaccine derived from clade 1 viruses will be effective against recent H5N1 strains in humans. This question was addressed in animal experiments using vaccine prepared from reverse genetics derived H5N1 (clade1) strains A/Hong Kong/213/03 (HK213/03) or A/Vietnam/JP1203/04 (VNJP1203/04) in the backbone of PR8 internal genes [43]. The resultant recombinant viruses, rgHK213/03 and rgVNJP1203/04, were tested in a mouse model. Mice immunised with rgHK213/03 (without or with 2% aluminium adjuvant) produced sufficient levels of serum antibodies that were cross-reactive to recent heterologous H5N1 isolates including A/Indonesia/6/05 (clade 2-subclade 1) and A/Turkey/12/06 (clade 2-subclade 2) and also elicited protective immunity against challenge with both homologous and heterologous wild-type H5N1 viruses. These immune responses were enhanced by addition of aluminium adjuvant, resulting in antigen sparing of vaccine. Mice immunised with rgVNJP1203/04 vaccine had low levels of serum antibodies and less protective immunity than that elicited with rgHK213/03 vaccine regardless of addition of aluminium adjuvant. A protective immunity induced by rgHK213/03 vaccine against challenge with homologous and heterologous H5N1 viruses was also observed in a ferret model although recent H5N1 isolates were not tested [44]. These studies suggest that rgHK213/03 vaccine is still useful as a backup vaccine for recent H5N1 viruses and if rgNJP1203/04 vaccine is employed, more vaccine would be necessary to induce sufficient immunity [43].
A cross-reactivity of whole-virus vaccine containing the HA gene of A/Duck/Singapore/3/97 (H5N3) in a genetic background of PR8 (Dk/Sing HA × PR/8) was tested in ferrets [45]. All animals vaccinated with Dk/Sing HA × PR/8 survived inoculation with a lethal dose of A/Vietnam/1203/04 (H5N1) (Viet/1203/04) virus. Immunised ferrets had significantly lower virus titres in the upper respiratory tract and clinically less severe disease. However, serum samples from animals immunised with Dk/Sing HA × PR/8 did not react with Viet/1203/04 in hemagglutination-inhibition or virus neutralisation test. These findings show that whole-virus H5 vaccines are cross-protective even if the HA is not antigenically matched to the challenge strain. In addition, neither hemagglutination-inhibition nor virus-neutralisation testing provides reliable correlates of cross protection in ferrets.
The results of animal experiments suggest that if vaccine derived from antigenically distinct viruses can induce protective immunity against coming pandemic viruses and if that efficacy last long enough, it will be possible to immunise naïve populations with viruses such as rgHK213/03 or Dk/Sing HA × PR/8 as a first-priming vaccines prior to a pandemic, and then boost with a vaccine produced from the pandemic strain. The use of such vaccine might help to solve the problem of timely development of an effective H5N1 vaccine from recently circulating H5N1 viruses in Southeast Asian countries. Moreover, although immunisation with such vaccines will not prevent morbidity, it is reasonable to expect that use of such vaccines will provide substantial protection and prevent mortality.
Inactivated subvirion or split vaccine
Split or subvirion vaccines are produced in the same way as whole virus vaccines, except the virus particles are disrupted using detergents (e.g. Triton X-100), or ethers in the past. Inactivated subvirion vaccine is generally safe and a danger of dilution or deviation of the protective immune responses after vaccination is decreased [28]. Seasonal influenza A subunit vaccine, which consists of purified HA and NA proteins (with the other viral components removed) causes fewer local reactions than a whole virus vaccine, and a single dose produces adequate antibody levels in a population exposed to similar viruses [46, 47]. However, it is believed that in a pandemic situation high antigen concentrations with inclusion of adjuvants and more than one dose will be required for unprimed population. These concerns may be of a special relevance for subunit vaccine because it is less immunogenic in immunologically naïve individuals compared to a whole-virus vaccine [41, 48, 49].
Faced with a pandemic threat posed by the Hong Kong H5N1 outbreak in 1997, the low-pathogenic avian influenza virus A/Duck/Singapore/97 (H5N3) was selected as a vaccine seed virus. The vaccine was developed as conventional HA surface-antigen preparation and assessed in a randomised phase I clinical trials [48, 50]. This vaccine revealed only poor immunogenicity at doses 7.5–30 μg even after two applications. Moreover, the H5N3 strain was not suitable for large scale vaccine production owing to its inefficient growth in eggs. The protective level of antibodies was achieved only when the vaccine was administered in combination with MF59 adjuvant. This adjuvanted vaccine candidate induced cross-reactive neutralising-antibody responses in humans to heterologous H5N1 viruses. Sera from immunised humans showed 100% cross-reactivity to H5N1 human viruses of 1997 (A/Hongkong/156/97 and A/HongKong/213/03), while cross-reactivity to viruses circulating in 2004 (A/Thailand/16/04 and A/Vietnam/1203/04) was lower: 71 and 43%, respectively [51]. These observations demonstrated a potential for use of such vaccine before an antigenically matched vaccine becomes available, thus suggesting that pre-pandemic priming of population might be a useful strategy even using subvirion vaccines [50, 51].
Several subvirion vaccines containing HA and NA from human H5N1 viruses were developed and evaluated in phase I clinical trials. In the USA, a dose ranging study of non-adjuvanted subvirion influenza A/Vietnam/1203/04 (H5N1) vaccine was done in healthy humans adults [52]. The seed virus prepared by reverse genetics contained HA (attenuated by modification at the cleavage site) and NA derived from the A/Vietnam/1203/04 and all other genes were derived from the PR8 virus. Although vaccine was well tolerated, only two doses each containing 90 μg HA (i.e. 12 times the seasonal influenza-vaccine dose) induced levels of antibody acceptable for licensing, achieving 54 and 58% seroconversions in neutralisation and hemagglutination-inhibition assay, respectively. Post-hoc analysis suggested that substantially higher responses occurred in recipients <40 years of age. This vaccine was recently approved by the FDA for immunisation of persons 18 through 64 years of age who are at increased risk of exposure to the H5N1 influenza virus subtype contained in the vaccine (see http://www.fda.gov/bbs/topics/NEWS/2007/NEW01611.html).
In another study involving 300 volunteers in France, split virion vaccine from the A/Vietnam/1194/04 in the backbone of PR8 virus was administered without or with aluminium hydroxide adjuvant. The vaccine induced an immune response consistent with European regulatory requirements for licensure only after two applications with 30 μg and adjuvant, achieving 67% hemagglutination inhibition seroconversion rate [49]. There was no adjuvant effect at doses of 7.5 or 15 μg haemagglutinin. Within current manufacturing constraints of split vaccine, supplies of the vaccine mentioned above would be limited to 75 or 225 million people only. In addition, egg yield of antigen from engineered H5N1 viruses are 30–40% lower than the average of seasonal viruses, reducing further the number of doses that would be available for clinical use [53]. Although these vaccines might be effective in preventing H5N1 influenza, other options that require much less HA are needed to overcome manufacturing limitations.
Novel approaches for the production HA for influenza vaccination have already been tested in humans. The production of purified HA can be performed by an expression in insect cells using a baculovirus expression vector. A baculovirus-based vaccine induced a better serum antibody response than a conventional vaccine against HA of H3 subtype [54, 55]. However, only modest immunogenicity in humans was demonstrated for vaccine prepared from recombinant H5 HA. Similar to trials with subvirion non-adjuvanted vaccine, two doses of baculovirus-based vaccine containing 90 μg purified HA were necessary to induce antibody titers in 52% of the recipients, while one dose was efficient only in 23% [56].
Live attenuated vaccine
A development of live attenuated influenza vaccine (LAIV) is based on the concept of cold-adaptation, or the growth of human influenza viruses at less than optimal temperatures, resulting in attenuation of a donor strain. The first LAIV against seasonal influenza was developed in Russia [57]. A similar LAIV (FluMist, MedImmune Vaccines) was licensed in the United States in 2003 for individuals from 5 to 49 years of age. The original cold-adapted virus strain was generated by serial passage at 25°C in tissue culture cells, which means that at normal human body temperature, it is attenuated. LAIV (FluMist) is made using cold-adapted A/Ann Arbor/6/60 (H2N2) and B/Ann Arbor/1/66 strains as genetic backbone into which HA and NA genes from circulating strains are inserted by genetic reassortment. The genetic stability of the attenuation phaenotype of the vaccine viruses results from changes in several of the backbone genes that reduce virulence [58, 59]. LAIV is usually administered by the natural way of infection, i.e., intranasally, providing antigen delivery to the submucosal immune cells of the nasopharyngeal-associated lymphoid tissue. A restriction of LAIV replication to the mucosa of the upper respiratory tract after intranasal inoculation limits its reactogenicity. LAIV induces serum IgG and nasal IgA antibodies as well as T cell response resulting in strong long-term local cellular and humoral responses, providing protection at the systemic and mucosal levels. After immunisation of healthy volunteers a protection was provided not only against the homologous strain but also against antigenically drifted influenza viruses [60]. Among young children, live attenuated vaccine had significantly better efficacy than inactivated vaccine. An evaluation of the risks and benefits indicates that live attenuated vaccine should be a highly effective, safe vaccine for children 12–59 months of age who do not have a history of asthma or wheezing [61]. Moreover, LAIV may stimulate immune response in influenza A virus-naïve individuals following a single dose of vaccine. These properties make LAIV attractive vaccines for the prevention of pandemic influenza in humans. The major concern linked with the LAIV is the possibility of genetic reversion (where the mutation causing attenuation change back to their wild-type state) and reassortment with wild-type influenza viruses, resulting in a new strain. However, administration of cold-adapted influenza A virus to humans at the time of wild-type virus infection suggested that LAIV is a safe procedure [62]. A recent study has also shown that no mutations occurred in any of nine LAIVs evaluated during the manufacturing process [63].
Reverse genetics based LAIVs possessing genes encoding a modified H5 HA and wild-type N1 from influenza A H5N1 viruses isolated in Hong Kong and Vietnam in 1997, 2003 and 2004, and remaining gene segments derived from cold-adapted influenza vaccine donor strain (A/Ann Arbor/6/60) were tested in mice and ferrets [64, 65]. The modified H5N1 cold-adapted candidate vaccine viruses were immunogenic in mice, attenuated in mice, ferrets and chicken, and protective against subsequent challenge with homologous and heterologous wild-type influenza viruses including A/Vietnam/JPHN0321/05 (clade1) and A/Indonesia/05/05 (clade 2-subclade 1) in mice and ferrets. The promising findings in preclinical studies of safety, immunogenicity, and efficacy of the H5N1 LAIV against antigenically diverse H5N1 viruses provide support for their evaluation in humans; clinical trials with prototype H5N1 viruses A/Vietnam/1203/04 and A/Hong Kong/492/97 are in progress (Med-Immune, USA).
A cross-protective efficacy of LAIV was also observed in animal experiments using H5 pandemic candidate created by classical reassortment techniques. The high growth reassortant virus Len/17/H5 contained H5 HA from a non-pathogenic avian influenza virus A/Duck/Pottsdam/1042–6/86 (H5N2) and other genes from cold-adapted attenuated A/Leningrad/134/17/57 (H2N2) strain. Mice administered Len/17/H5 either as a live-attenuated intranasal vaccine or as inactivated intramuscular vaccine were substantially protected from lethal challenge with highly pathogenic A/HongKong/483/97 and antigenically distinct A/Vietnam/1203/2004 [66, 67]. The cross-protective effect correlated with the levels of virus specific mucosal IgA and/or serum IgG antibodies [67]. These results support a general strategy of using classical genetic reassortment between a high-growth cold adapted H2N2 strain and antigenically related non-pathogenic avian viruses to prepare live-attenuated vaccines against multiple influenza A subtypes with pandemic potential.
DNA vaccines
Influenza DNA vaccines have attracted much attention since they were first reported to induce protective immune responses [47, 68, 69]. Virus DNA is uptaken by antigen presenting cells, which produce viral proteins in their cytosol. These viral proteins are then detected by the immune system, and trigger both humoral and cellular immune response. DNA vaccines are non-infectious, non replicating E. coli plasmids that encode only protein(s) of interest to which immune responses are induced. This feature makes it possible to vaccinate individuals multiple times without induction of immune-dampening vector specific responses. From a practical perspective, these vaccines may facilitate manufacturing [28]. The production of DNA vaccine in E. coli enables large-scale production and yields a highly pure and stable vaccine. A recent analysis has suggested that existing manufacturing technologies and infrastructure have the potential to provide DNA vaccines on a global scale [70].
Influenza DNA based vaccines induced protective and long-lasting haemagglutination inhibiting antibodies in different animal models and conferred protection against challenge with a homologous virulents strain of influenza A viruses in mice, chicken and ferrets [71–74]. DNA vaccine against conserved internal proteins, such as NP, generated CTL responses and conferred heterosubtypic immunity against lethal challenge [75]. This strategy has been also explored for possible H5N1 vaccine in a mouse model [76, 77]. DNA vaccine encoding HA from the influenza H5N1 isolate A/HongKong/156/97 (HK156) provided immunity against H5N1 infection of mice [78]. DNA vaccine encoding HA from A/Ty/Ir/1/83 (H5N8) virus, which differ from HK156 virus by 12% in HA1, prevented death but not H5N1 infection in mice [78]. DNA vaccination in mice with plasmids expressing conserved NP and M genes from an H1N1 protected against lethal challenge with HK156 virus. After HK156 exposure, mice survived rechallenge with A/Hong Kong/483/97, although the DNA vaccination alone protected poorly against this highly virulent strain. These results suggested that in the absence of antigenically matched HA-based vaccines, DNA vaccination with conserved influenza genes may provide a useful first line defence against a rapidly spreading pandemic virus. The initial results of a phase I study that evaluated intramuscular delivery of an influenza HA DNA vaccine trial were disappointing and data have not been formally released to assess the usefulness of this approach for next generation influenza vaccines. A promising strategy to improve DNA influenza vaccine may be a consensus-based approach [79]. This approach uses constructs designed by analysing a large number of circulating avian influenza viruses in order to generate a construct with the potential to induce highly cross-reactive cellular and humoral immune responses. By definition, these sequences should retain the most highly conserved regions, providing appropriate targets for immune responses. These constructs against H5N1 HA, NA and MX1 chosen from avian viruses isolated between 1997 and 2005 (for HA) and from both H1N1 and H5N1 (for NA and M1) were designed recently [79]. This DNA vaccine elicited strong CTL and humoral immune responses in mice and recombinant protein of H5 HA construct protected animals against lethal challenge with a highly pathogenic H5N1 strain (A/Hanoi/30408/05).
Viral vector based vaccine
Several viral vectors have been developed to deliver H5N1 virus DNA for vaccine purposes. Two replication defective adenoviral vectors expressing full-length H5 HA (derived from A/Hong Kong/156/97 or A/Vietnam/1203/04 strain) were tested in mice and poultry and, after two doses, were found to be immunogenic and protective against challenge with homologous and antigenically hetrologous H5N1 (clade 1) wild-type viruses [80, 81]. These vaccine candidates elicited both humoral and cellular immune responses, and the protection against heterologous challenge was presumed to be mediated by the cellular immune response. A major limitation for application of adenoviral vectors may be pre-existing immunity to human adenovirus, which could limit generation of immune response against a foreign gene of interest. However, available data from phase I and II clinical trials in humans with adenoviral-vector-based vaccine strategies did not indicate a limiting role of pre-existing immunity to adenoviruses and phase III trials are currently underway.
Other viral vectors tested for H5N1 vaccine involved poxvirus and New castle disease virus (NDV) vectors expressing H5 HA derived from avian virus A/turkey/Ireland/1378/83 (H5N8) and A/chicken/Italy/8/98 (H5N2), respectively [82, 83]. Moreover, NDV vaccine strain (LaSota) was used as vector for H5 HA form high pathogenic avian strain A/Bar-headed goose/Qinghai/3/2005 (H5N1) [84]. The poxvirus-vectored influenza vaccine showed immune responses against challenge with homologous and heterologous wild-type highly pathogenic H5N1 virus (AChicken/Indonesia/7/03) in a cat model [82]. NDV vectors protected chickens and mice from challenge with a lethal dose of homologous and heterologous highly pathogenic H5N1 viruses. The safety of NDV recombinants expressing protective antigens of respiratory human pathogens was recently demonstrated in two species of non-human primates after intranasal immunisation [85].
Virus-vector-based vaccines may be delivered by either a parenteral or topical (mucosal) route and may provide the advantage of inducing strong humoral and cellular immunity and conferring cross-protection against continuously evolving H5N1 viruses. In addition, virus-vector-based delivery systems elicit strong immune responses without adjuvant applications and the production of some vectors (e.g. vectors derived from adenovirus) is egg-independent. Although this type of vaccine was designed mostly for immunisation of poultry, it may also have potential use in high-risk human individuals to control the pandemic spread of lethal avian influenza.
Live influenza virus vaccine with altered NS1 gene
A rational approach to the generation of live viral vaccine was proposed by using influenza viruses that possess altered viral non-structural protein 1 (NS1), the main antagonist of the interferon (IFN) response of the host [86, 87]. By reverse genetics it became possible to construct NS1 deleted viruses, which were not able to replicate in IFN competent cells. It was shown that influenza A and B viruses encoding altered viral NS1 proteins were both highly attenuated in the mouse host, and provided adequate protection from challenge with wild-type virus [88]. In addition, viruses lacking functional NS1 protein produce high level of IFN and other cytokines that are responsible for the increased immunogenicity of such viruses [89]. Expression of endogenous IFN appears to be excellent adjuvant that enhances production of immunoglobulins and contribute to the activation of DCs required for antigen presentation [90, 91]. It was suggested that using live attenuated vaccine with deleted NS1 protein would cause enhanced immune response compared to that of conventional live or killed vaccine. This process should translate into lower doses of live virus vaccine required to induce a robust and protective immune response. This makes this approach highly attractive in the light of a possible pandemic. Reverse genetics technology enables to use NS1 deleted influenza virus as seed virus for H5N1 vaccine (Fig. 1). Clinical phase I studies are in progress to determine a safety and immunogenicity of vaccine derived from NS1 deleted influenza A virus (PR8 strain) (Avir Green Hills Biotechnology AG, Vienna, Austria).
Universal influenza virus vaccine
An ideal influenza vaccine would be effective against a range of virus subtypes and could be useful during pandemic and interpandemic periods. Several attempts were made to prepare such universal vaccine using influenza proteins that are conserved among different subtypes and exert low mutation rate. A most promising approach was based on using ectodomain of the M2 protein (M2e), which exerts a high degree of conservation amongst human influenza A virus strains [92]. The M2e protein induced cross-reactive immunity that in turn resulted in less severe disease in animal models after challenge with wild-type virus [93, 94]. Similarly, immunisation with the NA antigen is likely to induce responses that are more cross-reactive than those by the more variable HA [95]. However, both M2 and NA specific antibodies are not protective in infected humans, because they do not prevent influenza virus infection. However, they may reduce viral spread and thereby accelerate the recovery from influenza.
There is convincing evidence that M2e-specific antibody-mediated protection is currently lacking or is suboptimal in humans presenting with naturally acquired influenza A virus infection [96, 97]. This provides a strong incentive for the development of an M2e-specific vaccine. Several companies are working on the commercialisation of an M2-based vaccine. It was shown that M2e conjugated to keyhole limpet hemocyanin or Neisseria meningitides outer membrane protein complex (Merck, USA) or particles containing M2e peptide linked to the hepatitis B virus core subunit (Acambis, USA and Cytos Biotechnology, Switzerland) significantly enhanced the immune response, reduced the number of vaccinations required for complete protection against a lethal challenge with different influenza A strains and significantly reduced morbidity in animal models [98–100].
Cell culture-grown influenza vaccine
Currently marketed inactivated influenza vaccines are produced in embryonic hen’s eggs. Approximately 250 million doses are brought to market annually in over 100 countries. In addition to the tight timeline necessitated by the vaccine strain selection process, the supply of high quality fertilised eggs must be carefully timed well in advance to provide sufficient capacity for vaccine manufacture [101]. The cell-based technology is an alternative process that offers several advantages especially for a pandemic situation. The cell manufacturing process will be more rapid, better controlled and more easily increased for large-scale vaccine production. Growth of virus in serum-free or even protein-free cell culture [102] significantly minimises the risk for microbial contamination or potential allergic reactions to egg components. Influenza viruses grown in mammalian cell culture were shown to be more similar to those in human clinical specimens compared with their egg-grown counterparts [103, 104]. Inactivated vaccine prepared from the virus grown in mammalian cells induced more cross-reactive serum antibodies and revealed better protection than vaccine made from egg-grown viruses [105]. Two mammalian cell lines, Madin–Darby canine kidney (MDCK) and the African green monkey kidney (Vero) cell lines are already approved in several countries for the production of inactivated vaccine. Another mammalian cell line, PER.C6, is also under consideration as a substrate for influenza vaccine [106]. The PER.C6 cell line is a human fetal retinoblasts immortalised by transfection with E1 minigene of adenovirus type 5. Clinical trials with H5N1 surface antigen pandemic vaccine produced in MDCK cell line (Solvay Pharmaceuticals, Netherlands) and with a whole virion vaccine produced in Vero cell line (Baxter, Austria) have been initiated in 2006. Clinical trials with H7N7 vaccine in PERC.C6 cell line has been undertaken in the UK (Sanofi Pasteur).
Conclusion
Several phase I clinical studies with inactivated whole-virus or split vaccines against different H5 viruses have demonstrated only limited efficacy when compared with the seasonal influenza vaccine. To induce protective immunity in unprimed individuals two immunisations with at least the double amount of H5N1 vaccine, mostly with adjuvant inclusion, were required. These findings demonstrate that under the circumstances of a pandemic, the amount of inactivated vaccine will be several times higher, and time required for efficient protection, will be twice longer than with the seasonal influenza vaccine. Cell culture-based technology holds promise to improve production and manufacturing of pandemic vaccines. Although cross-reactivity has been shown with reverse-genetics-based H5N1 vaccines in animal models, it is not known whether such cross-reactivity extends to humans. The impact of antigenic diversity of avian influenza viruses for stockpiling of pandemic vaccine appears to be that more than one, and possibly multiple, current vaccines are needed. These findings raise concerns regarding production capacity, global accessibility and manufacturing costs associated with a pandemic situation. Novel strategies for the development of vaccines that are egg-independent and adjuvant-independent, broadly cross-reactive and long-lasting are highly desirable.
References
Webster RG, Govorkova EA (2006) H5N1 influenza—continuing evolution and spread. N Engl J Med 335:2174–2177
Cinatl J Jr, Michaelis M, Doerr HW (2007) The threat of avian influenza a (H5N1). Part I: epidemiologic concerns and virulence determinants. Med Microbiol Immunol. 2007 [Epub ahead of print]
Cinatl J Jr, Michaelis M, Doerr HW (2007) The threat of avian influenza a (H5N1). Part II: clues to pathogenicity and pathology. Med Microbiol Immunol. 2007 [Epub ahead of print]
The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5 (2005) Avian influenza A (H5N1) infection in humans. N Engl J Med 353:1374–1385
Schunemann HJ, Hill SR, Kakad M, Bellamy R, Uyeki TM, Hayden FG, Yazdanpanah Y, Beigel J, Chotpitayasunondh T, Del Mar C, Farrar J, Tran TH, Ozbay B, Sugaya N, Fukuda K, Shindo N, Stockman L, Vist GE, Croisier A, Nagjdaliyev A, Roth C, Thomson G, Zucker H, Oxman AD, WHO Rapid Advice Guideline Panel on Avian Influenza (2007) WHO rapid advice guidelines for pharmacological management of sporadic human infection with avian influenza A (H5N1) virus. Lancet Infect Dis 7:21–31
Cinatl J Jr, Michaelis M, Doerr HW (2007) The threat of avian influenza A (H5N1). Part III: antiviral therapy. Med Microbiol Immunol 2007 [Epub ahead of print]
World Health Organization (2006) Antigenic and genetic characteristics of H5N1 viruses and H5N1 vaccine viruses developed for potential use as pre-pandemic vaccine. Wkly Epidemiol Rec 81(34/35):328–330
Subbarao K, Murphy BR, Fauci AS (2006) Development of effective vaccines against pandemic influenza. Immunity 24:5–9
Stephenson I, Gust I, Pervikov Y, Kieny MP (2006) Development of vaccines against influenza H5. Lancet Infect Dis 6:458–460
Subbarao K, Luke C (2007) H5N1 viruses and vaccines. PLoS Pathog 3:e40
Johansson BE, Bucher DJ, Kilbourne ED (1989) Purified influenza virus hemagglutinin and neuraminidase are equivalent in stimulation of antibody response but induce contrasting types of immunity to infection. J Virol 63:1239–1246
Tamura S, Tanimoto T, Kurata T (2005) Mechanisms of broad cross-protection provided by influenza virus infection and their application to vaccines. Jpn J Infect Dis 58:195–207
Powers DC, Kilbourne ED, Johansson BE (1996) Neuraminidase-specific antibody responses to inactivated influenza virus vaccine in young and elderly adults. Clin Diagn Lab Immunol 3:511–516
Black RA, Rota PA, Gorodkova N, Klenk HD, Kendal AP (1993) Antibody response to the M2 protein of influenza A virus expressed in insect cells. J Gen Virol 74:143–146
Murphy BR, Clements ML (1989) The systemic and mucosal immune response of humans to influenza A virus. Curr Top Microbiol Immunol 146:107–116
McMichael AJ, Gotch FM, Noble GR, Beare PA (1983) Cytotoxic T-cell immunity to influenza. N Engl J Med 309:13–17
Bender BS, Croghan T, Zhang L, Small PA Jr (1992) Transgenic mice lacking class I major histocompatibility complex-restricted T cells have delayed viral clearance and increased mortality after influenza virus challenge. J Exp Med 175:1143–1145
Yewdell JW, Bennink JR, Smith GL, Moss B (1985) Influenza A virus nucleoprotein is a major target antigen for cross-reactive anti-influenza A virus cytotoxic T lymphocytes. Proc Natl Acad Sci USA 82:1785–1789
Wang M, Lamberth K, Harndahl M, Roder G, Stryhn A, Larsen MV, Nielsen M, Lundegaard C, Tang ST, Dziegiel MH, Rosenkvist J, Pedersen AE, Buus S, Claesson MH, Lund O (2007) CTL epitopes for influenza A including the H5N1 bird flu; genome-, pathogen-, and HLA-wide screening. Vaccine 25(15):2823–2831
Jameson J, Cruz J, Ennis FA (1998) Human cytotoxic T-lymphocyte repertoire to influenza A viruses. J Virol 72:8682–8689
Nakajima K, Desselberger U, Palese P (1978) Recent human influenza A (H1N1) viruses are closely related genetically to strains isolated in 1950. Nature 274:334–339
Horimoto T, Kawaoka Y (2006) Strategies for developing vaccines against H5N1 influenza A viruses. Trends Mol Med 12:506–514
Couch RB, Kasel JA (1983) Immunity to influenza in man. Annu Rev Microbiol 37:529–549
Epstein SL (2006) Prior H1N1 influenza infection and susceptibility of Cleveland Family Study participants during the H2N2 pandemic of 1957: an experiment of nature. J Infect Dis 193:49–53
Murphy BR, Kasel JA, Chanock RM (1972) Association of serum anti-neuraminidase antibody with resistance to influenza in man. N Engl J Med 286:1329–1332
Gillim-Ross L, Subbarao K (2007) Can immunity induced by the human influenza virus N1 neuraminidase provide some protection from Avian Influenza H5N1 Viruses? PLoS Med 4:e91
Sandbulte MR, Jimenez GS, Boon AC, Smith LR, Treanor JJ, Webby RJ (2007) Cross-reactive neuraminidase antibodies afford partial protection against H5N1 in mice and are present in unexposed humans. PLoS Med 4:e59
Ulmer JB, Valley U, Rappuoli R (2006) Vaccine manufacturing: challenges and solutions. Nat Biotechnol 24:1377–1383
Hehme N, Engelmann H, Kunzel W, Neumeier E, Sanger R (2002) Pandemic preparedness: lessons learnt from H2N2 and H9N2 candidate vaccines. Med Microbiol Immunol 191:203–208
Hehme N, Engelmann H, Kuenzel W, Neumeier E, Saenger R (2004) Immunogenicity of a monovalent, aluminum-adjuvanted influenza whole virus vaccine for pandemic use. Virus Res 103:163–171
Nonacs R, Humborg C, Tam JP, Steinman RM (1992) Mechanisms of mouse spleen dendritic cell function in the generation of influenza-specific, cytolytic T lymphocytes. J Exp Med 176:519–529
Bhardwaj N, Bender A, Gonzalez N, Bui LK, Garrett MC, Steinman RM (1994) Influenza virus-infected dendritic cells stimulate strong proliferative and cytolytic responses from human CD8+ T cells. J Clin Invest 94:797–807
Heath WR, Carbone FR (2001) Cross-presentation in viral immunity and self-tolerance. Nat Rev Immunol 1:126–134
Takada A, Kuboki N, Okazaki K, Ninomiya A, Tanaka H, Ozaki H, Itamura S, Nishimura H, Enami M, Tashiro M, Shortridge KF, Kida H (1999) Avirulent Avian influenza virus as a vaccine strain against a potential human pandemic. J Virol 73:8303–8307
Webby RJ, Perez DR, Coleman JS, Guan Y, Knight JH, Govorkova EA, McClain-Moss LR, Peiris JS, Rehg JE, Tuomanen EI, Webster RG (2004) Responsiveness to a pandemic alert: use of reverse genetics for rapid development of influenza vaccines. Lancet 363:1099–1103
Wood JM, Robertson JS (2004) From lethal virus to life-saving vaccine: developing inactivated vaccines for pandemic influenza. Nat Rev Microbiol 2:842–847
Horimoto T, Takada A, Fujii K, Goto H, Hatta M, Watanabe S, Iwatsuki-Horimoto K, Ito M, Tagawa-Sakai Y, Yamada S, Ito H, Ito T, Imai M, Itamura S, Odagiri T, Tashiro M, Lim W, Guan Y, Peiris M, Kawaoka Y (2006) The development and characterization of H5 influenza virus vaccines derived from a 2003 human isolate. Vaccine 24:3669–3676
Nicolson C, Major D, Wood JM, Robertson JS (2005) Generation of influenza vaccine viruses on Vero cells by reverse genetics: an H5N1 candidate vaccine strain produced under a quality system. Vaccine 23:2943–2952
Horimoto T, Kawaoka Y (2005) Influenza: lessons from past pandemics, warnings from current incidents. Nat Rev Microbiol 3:591–600
Lin J, Zhang J, Dong X, Fang H, Chen J, Su N, Gao Q, Zhang Z, Liu Y, Wang Z, Yang M, Sun R, Li C, Lin S, Ji M, Liu Y, Wang X, Wood J, Feng Z, Wang Y, Yin W (2006) Safety and immunogenicity of an inactivated adjuvanted whole-virion influenza A (H5N1) vaccine: a phase I randomised controlled trial. Lancet 368:991–997
Nicholson KG, Tyrrell DA, Harrison P, Potter CW, Jennings R, Clark A, Schild GC, Wood JM, Yetts R, Seagroatt V, Huggins A, Anderson SG (1979) Clinical studies of monovalent inactivated whole virus and subunit A/USSR/77 (H1N1) vaccine: serological responses and clinical reactions. J Biol Stand 7:123–136
Wright PF, Thompson J, Vaughn WK, Folland DS, Sell SH, Karzon DT (1977) Trials of influenza A/New Jersey/76 virus vaccine in normal children: an overview of age-related antigenicity and reactogenicity. J Infect Dis 136(Suppl):S731–S741
Ninomiya A, Imai M, Tashiro M, Odagiri T (2007) Inactivated influenza H5N1 whole-virus vaccine with aluminum adjuvant induces homologous and heterologous protective immunities against lethal challenge with highly pathogenic H5N1 avian influenza viruses in a mouse model. Vaccine 25(18):3554–3560
Govorkova EA, Webby RJ, Humberd J, Seiler JP, Webster RG (2006) Immunization with reverse-genetics-produced H5N1 influenza vaccine protects ferrets against homologous and heterologous challenge. J Infect Dis 194:159–167
Lipatov AS, Hoffmann E, Salomon R, Yen HL, Webster RG (2006) Cross-protectiveness and immunogenicity of influenza A/Duck/Singapore/3/97(H5) vaccines against infection with A/Vietnam/1203/04(H5N1) virus in ferrets. J Infect Dis 194:1040–1043
Couch RB, Keitel WA, Cate TR (1997) Improvement of inactivated influenza virus vaccines. J Infect Dis 176(Suppl 1):S38–S44
Hilleman MR (2002) Realities and enigmas of human viral influenza: pathogenesis, epidemiology and control. Vaccine 20:3068–3087
Stephenson I, Nicholson KG, Wood JM, Zambon MC, Katz JM (2004) Confronting the avian influenza threat: vaccine development for a potential pandemic. Lancet Infect Dis 4:499–509
Bresson JL, Perronne C, Launay O, Gerdil C, Saville M, Wood J, Hoschler K, Zambon MC (2006) Safety and immunogenicity of an inactivated split-virion influenza A/Vietnam/1194/2004 (H5N1) vaccine: phase I randomised trial. Lancet 367:1657–1664
Nicholson KG, Colegate AE, Podda A, Stephenson I, Wood J, Ypma E, Zambon MC (2001) Safety and antigenicity of non-adjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet 357:1937–1943
Stephenson I, Bugarini R, Nicholson KG, Podda A, Wood JM, Zambon MC, Katz JM (2005) Cross-reactivity to highly pathogenic avian influenza H5N1 viruses after vaccination with nonadjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a potential priming strategy. J Infect Dis 191:1210–1215
Treanor JJ, Campbell JD, Zangwill KM, Rowe T, Wolff M (2006) Safety and immunogenicity of an inactivated subvirion influenza A (H5N1)vaccine. N Engl J Med 2354:1343–1351
Stephenson I (2006) H5N1 vaccines: how prepared are we for a pandemic? Lancet 368:965–966
Treanor JJ, Schiff GM, Couch RB, Cate TR, Brady RC, Hay CM, Wolff M, She D, Cox MM (2006) Dose-related safety and immunogenicity of a trivalent baculovirus-expressed influenza-virus hemagglutinin vaccine in elderly adults. J Infect Dis 193:1223–1228
Wang K, Holtz KM, Anderson K, Chubet R, Mahmoud W, Cox MM (2006) Expression and purification of an influenza hemagglutinin—one step closer to a recombinant protein-based influenza vaccine. Vaccine 24:2176–2185
Treanor JJ, Wilkinson BE, Masseoud F, Hu-Primmer J, Battaglia R, O’Brien D, Wolff M, Rabinovich G, Blackwelder W, Katz JM (2001) Safety and immunogenicity of a recombinant hemagglutinin vaccine for H5 influenza in humans. Vaccine 19:1732–1737
Kendal AP (1997) Cold-adapted live attenuated influenza vaccines developed in Russia: can they contribute to meeting the needs for influenza control in other countries? Eur J Epidemiol 13:591–609
Jin H, Lu B, Zhou H, Ma C, Zhao J, Yang CF, Kemble G, Greenberg H (2003) Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18–24
Hoffmann E, Mahmood K, Chen Z, Yang CF, Spaete J, Greenberg HB, Herlocher ML, Jin H, Kemble G (2005) Multiple gene segments control the temperature sensitivity and attenuation phenotypes of ca B/Ann Arbor/1/66. J Virol 79:11014–11021
Belshe RB, Nichol KL, Black SB, Shinefield H, Cordova J, Walker R, Hessel C, Cho I, Mendelman PM (2004) Safety, efficacy, and effectiveness of live, attenuated, cold-adapted influenza vaccine in an indicated population aged 5–49 years. Clin Infect Dis 39:920–927
Belshe RB, Edwards KM, Vesikari T, Black SV, Walker RE, Hultquist M, Kemble G, Connor EM; CAIV-T Comparative Efficacy Study Group (2007) Live attenuated versus inactivated influenza vaccine in infants and young children. N Engl J Med 356:685–696
Youngner JS, Treanor JJ, Betts RF, Whitaker-Dowling P (1994) Effect of simultaneous administration of cold-adapted and wild-type influenza A viruses on experimental wild-type influenza infection in humans. J Clin Microbiol 32:750–754
Buonagurio DA, Bechert TM, Yang CF, Shutyak L, D’Arco GA, Kazachkov Y, Wang HP, Rojas EA, O’Neill RE, Spaete RR, Coelingh KL, Zamb TJ, Sidhu MS, Udem SA (2006) Genetic stability of live, cold-adapted influenza virus components of the FluMist/CAIV-T vaccine throughout the manufacturing process. Vaccine 24:2151–2160
Li S, Liu C, Klimov A, Subbarao K, Perdue ML, Mo D, Ji Y, Woods L, Hietala S, Bryant M (1999) Recombinant influenza A virus vaccines for the pathogenic human A/Hong Kong/97 (H5N1) viruses. J Infect Dis 179:1132–1138
Suguitan AL Jr, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, Luke CJ, Murphy B, Swayne DE, Kemble G, Subbarao K (2006) Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med 3:e360
Lu X, Edwards LE, Desheva JA, Nguyen DC, Rekstin A, Stephenson I, Szretter K, Cox NJ, Rudenko LG, Klimov A, Katz JM (2006) Cross-protective immunity in mice induced by live-attenuated or inactivated vaccines against highly pathogenic influenza A (H5N1) viruses. Vaccine 24:6588–6593
Desheva JA, Lu XH, Rekstin AR, Rudenko LG, Swayne DE, Cox NJ, Katz JM, Klimov AI (2006) Characterization of an influenza A H5N2 reassortant as a candidate for live-attenuated and inactivated vaccines against highly pathogenic H5N1 viruses with pandemic potential. Vaccine 24:6859–6866
Ada G, Ramshaw I (2003) DNA vaccination. Expert Opin Emerg Drugs 8:27–35
Ulmer JB (2002) Influenza DNA vaccines. Vaccine 20(Suppl 2):S74–S76
Hoare M, Levy MS, Bracewell DG, Doig SD, Kong S, Titchener-Hooker N, Ward JM, Dunnill P (2005) Biprocess engineering issues that would be faced in producing a DNA vaccine at up to 100m3 fermentation scale for an influenza pandemic. Biotechnol Prog 21:1577–1592
Liu MA, McClements W, Ulmer JB, Shiver J, Donnelly J (1997) Immunization of non-human primates with DNA vaccines. Vaccine 15:909–912
Pertmer TM, Eisenbraun MD, McCabe D, Prayaga SK, Fuller DH, Haynes JR (1995) Gene gun-based nucleic acid immunization: elicitation of humoral and cytotoxic T lymphocyte responses following epidermal delivery of nanogram quantities of DNA. Vaccine 13:1427–1430
Robinson HL, Hunt LA, Webster RG (1993) Protection against a lethal influenza virus challenge by immunization with a haemagglutinin-expressing plasmid DNA. Vaccine 11:957–960
Ulmer JB, Fu TM, Deck RR, Friedman A, Guan L, DeWitt C, Liu X, Wang S, Liu MA, Donnelly JJ, Caulfield MJ (1998) Protective CD4+ and CD8+ T cells against influenza virus induced by vaccination with nucleoprotein DNA. J Virol 72:5648–5653
Ulmer JB, Donnelly JJ, Parker SE, Rhodes GH, Felgner PL, Dwarki VJ, Gromkowski SH, Deck RR, DeWitt CM, Friedman A et al (1993) Heterologous protection against influenza by injection of DNA encoding a viral protein. Science 259:1745–1749
Kodihalli S, Kobasa DL, Webster RG (2000) Strategies for inducing protection against avian influenza A virus subtypes with DNA vaccines. Vaccine 18:2592–2599
Epstein SL, Tumpey TM, Misplon JA, Lo CY, Cooper LA, Subbarao K, Renshaw M, Sambhara S, Katz JM (2002) DNA vaccine expressing conserved influenza virus proteins protective against H5N1 challenge infection in mice. Emerg Infect Dis 8:796–801
Kodihalli S, Goto H, Kobasa DL, Krauss S, Kawaoka Y, Webster RG (1999) DNA vaccine encoding hemagglutinin provides protective immunity against H5N1 influenza virus infection in mice. J Virol 73:2094–2098
Laddy DJ, Yan J, Corbitt N, Kobasa D, Kobinger GP, Weiner DB (2007) Immunogenicity of novel consensus-based DNA vaccines against avian influenza. Vaccine 25(16):2984–2989
Gao W, Soloff AC, Lu X, Montecalvo A, Nguyen DC, Matsuoka Y, Robbins PD, Swayne DE, Donis RO, Katz JM, Barratt-Boyes SM, Gambotto A (2006) Protection of mice and poultry from lethal H5N1 avian influenza virus through adenovirus-based immunization. J Virol 80:1959–1964
Hoelscher MA, Garg S, Bangari DS, Belser JA, Lu X, Stephenson I, Bright RA, Katz JM, Mittal SK, Sambhara S (2006) Development of adenoviral-vector-based pandemic influenza vaccine against antigenically distinct human H5N1 strains in mice. Lancet 367:475–481
Karaca K, Swayne DE, Grosenbaugh D, Bublot M, Robles A, Spackman E, Nordgren R (2005) Immunogenicity of fowlpox virus expressing the avian influenza virus H5 gene (TROVAC AIV-H5) in cats. Clin Diagn Lab Immunol 12:1340–1342
Veits J, Wiesner D, Fuchs W, Hoffmann B, Granzow H, Starick E, Mundt E, Schirrmeier H, Mebatsion T, Mettenleiter TC, Romer-Oberdorfer A (2006) Newcastle disease virus expressing H5 hemagglutinin gene protects chickens against Newcastle disease and avian influenza. Proc Natl Acad Sci USA 103:8197–8202
Ge J, Deng G, Wen Z, Tian G, Wang Y, Shi J, Wang X, Li Y, Hu S, Jiang Y, Yang C, Yu K, Bu Z, Chen H (2007) Newcastle disease virus-based live attenuated vaccine completely protects chickens and mice from lethal challenge of homologous and heterologous H5N1 avian influenza viruses. J Virol 81:150–158
Bukreyev A, Huang Z, Yang L, Elankumaran S, St Claire M, Murphy BR, Samal SK, Collins PL (2005) Recombinant newcastle disease virus expressing a foreign viral antigen is attenuated and highly immunogenic in primates. J Virol 79:13275–13284
Egorov A, Brandt S, Sereinig S, Romanova J, Ferko B, Katinger D, Grassauer A, Alexandrova G, Katinger H, Muster T (1998) Transfectant influenza A viruses with long deletions in the NS1 protein grow efficiently in Vero cells. J Virol 72:6437–6441
Garcia-Sastre A, Egorov A, Matassov D, Brandt S, Levy DE, Durbin JE, Palese P, Muster T (1998) Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology 252:324–330
Talon J, Salvatore M, O’Neill RE, Nakaya Y, Zheng H, Muster T, Garcia-Sastre A, Palese P (2000) Influenza A and B viruses expressing altered NS1 proteins: A vaccine approach. Proc Natl Acad Sci USA 97:4309–4314
Ferko B, Stasakova J, Romanova J, Kittel C, Sereinig S, Katinger H, Egorov A (2004) Immunogenicity and protection efficacy of replication-deficient influenza A viruses with altered NS1 genes. J Virol 78:13037–13045
Proietti E, Bracci L, Puzelli S, Di Pucchio T, Sestili P, De Vincenzi E, Venditti M, Capone I, Seif I, De Maeyer E, Tough D, Donatelli I, Belardelli F (2002) Type I IFN as a natural adjuvant for a protective immune response: lessons from the influenza vaccine model. J Immunol 169:375–383
Bracci L, Canini I, Puzelli S, Sestili P, Venditti M, Spada M, Donatelli I, Belardelli F, Proietti E (2005) Type I IFN is a powerful mucosal adjuvant for a selective intranasal vaccination against influenza virus in mice and affects antigen capture at mucosal level. Vaccine 23:2994–3004
Neirynck S, Deroo T, Saelens X, Vanlandschoot P, Jou WM, Fiers W (1999) A universal influenza A vaccine based on the extracellular domain of the M2 protein. Nat Med 5:1157–1163
Ernst WA, Kim HJ, Tumpey TM, Jansen AD, Tai W, Cramer DV, Adler-Moore JP, Fujii G (2006) Protection against H1, H5, H6 and H9 influenza A infection with liposomal matrix 2 epitope vaccines. Vaccine 24:5158–5168
Gerhard W (2006) Influenza A virus infection engenders a poor antibody response against the ectodomain of matrix protein 2. Virol J 3:102
Kilbourne ED, Couch RB, Kasel JA, Keitel WA, Cate TR, Quarles JH, Grajower B, Pokorny BA, Johansson BE (1995) Purified influenza A virus N2 neuraminidase vaccine is immunogenic and non-toxic in humans. Vaccine 13:1799–1803
Johansson BE, Kilbourne ED (1993) Dissociation of influenza virus hemagglutinin and neuraminidase eliminates their intravirionic antigenic competition. J Virol 67:5721–5723
Feng J, Zhang M, Mozdzanowska K, Zharikova D, Hoff H, Wunner W, Couch RB, Gerdil C (2003) The annual production cycle for influenza vaccine. Vaccine 21:1776–1779
De Filette M, Ramne A, Birkett A, Lycke N, Lowenadler B, Min Jou W, Saelens X, Fiers W (2006) The universal influenza vaccine M2e-HBc administered intranasally in combination with the adjuvant CTA1-DD provides complete protection. Vaccine 24:544–551
Fan J, Liang X, Horton MS, Perry HC, Citron MP, Heidecker GJ, Fu TM, Joyce J, Przysiecki CT, Keller PM, Garsky VM, Ionescu R, Rippeon Y, Shi L, Chastain MA, Condra JH, Davies ME, Liao J, Emini EA, Shiver JW (2004) Preclinical study of influenza virus A M2 peptide conjugate vaccines in mice, ferrets, and rhesus monkeys. Vaccine 22:2993–3003
Jegerlehner A, Schmitz N, Storni T, Bachmann MF (2004) Influenza A vaccine based on the extracellular domain of M2: weak protection mediated via antibody-dependent NK cell activity. J Immunol 172:5598–5605
Gerdil C (2003) The annual production cycle for influenza vaccine. Vaccine 21:1776–1779
Cinatl J Jr, Cinatl J, Rabenau H, Rapp J, Kornhuber B, Doerr HW (1993) Protein-free culture of Vero cells: a substrate for replication of human pathogenic viruses. Cell Biol Int 17:885–895
Katz JM, Wang M, Webster RG (1990) Direct sequencing of the HA gene of influenza (H3N2) virus in original clinical samples reveals sequence identity with mammalian cell-grown virus. J Virol 64:1808–1811
Schild GC, Oxford JS, de Jong JC, Webster RG (1983) Evidence for host-cell selection of influenza virus antigenic variants. Nature 303:706–709
Alymova IV, Kodihalli S, Govorkova EA, Fanget B, Gerdil C, Webster RG (1998) Immunogenicity and protective efficacy in mice of influenza B virus vaccines grown in mammalian cells or embryonated chicken eggs. J Virol 72:4472–4477
Pau MG, Ophorst C, Koldijk MH, Schouten G, Mehtali M, Uytdehaag F (2001) The human cell line PER.C6 provides a new manufacturing system for the production of influenza vaccines. Vaccine 19:2716–2721
Acknowledgments
The authors thank Rouslan Kotchetkov for critical reading of the manuscript. The authors have been supported by the European Commission-funded projects LSH-CT-2004–512054 (Contract Number: 512054) and COOP-CT-2004 (Contract Number: 512864).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cinatl jr, J., Michaelis, M. & Doerr, H.W. The threat of avian influenza A (H5N1). Part IV: development of vaccines. Med Microbiol Immunol 196, 213–225 (2007). https://doi.org/10.1007/s00430-007-0052-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-007-0052-3