Abstract
Purpose of Review
The role of retrograde hindfoot nailing in the treatment of acute orthopedic trauma is explored.
Recent Findings
Tibio-talar calcaneal (TTC) nailing is an acceptable treatment alternative for the low-demand geriatric patient with peri-articular ankle trauma permitting immediate weight-bearing with low rates of complication and return to functionality. Hindfoot nailing can be used for limb salvage in the younger active patient; yet, joint-preserving reconstruction is preferred when feasible.
Summary
Retrograde TTC nailing is a reliable option for hindfoot/distal tibia stabilization especially in the elderly frail population. Hindfoot nailing is reserved for a select subset of active patients when severity of bone, joint, and soft tissue injury are not amenable to more conventional reconstruction.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rammelt S, Pyrc J, Agren PH, Hartsock LA, Cronier P, Friscia DA, et al. Tibiotalocalcaneal fusion using the hindfoot arthrodesis nail: a multicenter study. Foot Ankle Int. 2013;34(9):1245–55.
Loosen S, Preuss S, Zelle BA, Pape HC, Tarkin IS. Multimorbid patients with poor soft tissue conditions: treatment of distal tibia fractures with retrograde intramedullary nailing. Unfallchirurg. 2013;116(6):553–8.
Lemon M, Somayaji HS, Khaleel A, Elliott DS. Fragility fractures of the ankle: stabilisation with an expandable calcaneotalotibial nail. J Bone Joint Surg Br. 2005;87(6):809–13. In one of the earliest published examples of an acutely applied tibiotalocalcaneal nail in fracture management, the authors describe the use of an expandable nail to fuse the subtalar and tibiotalar joints in geriatric patients with fragility injuries. Weight-bearing was permitted immediately after surgery, and no wound issues were reported. Part of the proposed protocol included nail removal to avoid periprosthetic fractures, although this was declined by a significant percentage of patients. However, no periprosthetic injuries were reported regardless.
Amirfeyz R, Bacon A, Ling J, Blom A, Hepple S, Winson I, et al. Fixation of ankle fragility fractures by tibiotalocalcaneal nail. Arch Orthop Trauma Surg. 2008;128(4):423–8. Thirteen patients were treated with either a long humeral nail or a short TTC fusion nail through the same approach. All patients returned to their baseline function regardless of the hardware used, and radiographic analysis showed fracture union in all cases. Findings reinforced that the benefits of TTC nailing, early weight-bearing, and fewer complications outweighed the stiffness that resulted from the joint immobilization in the geriatric population.
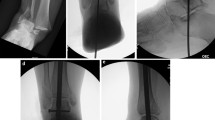
Fourman MS, Tarkin IS. Retrograde tibiotalocalcaneal hindfoot nail without joint preparation is a viable salvage technique for geriatrics with extensive comorbidities and minimal ambulatory status following major trauma Proceedings of the American Academy of Orthopaedic Surgery Annual Meeting; Orlando, FL; March 2017. Here, we describe our institutional experience with acute TTC nailing following orthopedic trauma, which included a total of 18 patients treated after high- and low-energy injuries. Joint preparation was only performed in those patients whose traumatic wounds permitted access. Despite a significantly co-morbid population (mean Charlson Index 3.9) and a high percentage (22.2%) of high-energy trauma, limb preservation was possible in 88.9% of patients, and 83.3% were able to return to weight-bearing as tolerated.
Jonas SC, Young AF, Curwen CH, McCann PA. Functional outcome following tibio-talar-calcaneal nailing for unstable osteoporotic ankle fractures. Injury. 2013;44(7):994–7. A short TTC nail was used to stabilize the ankles of 31 patients after a low-energy fragility fracture. Like prior work, the authors reported a 93.5% return to baseline mobility rate. However, five nail complications (3 fractures, 2 nail failures) that required re-operation were reported, which raised the question of patient candidacy vs. nail biomechanical advantage. The authors hypothesized that active patients must be watched closely for hardware failure.
Al-Nammari SS, Amin A, Nielsen D. Fragility fractures of the ankle in the frail elderly patient: treatment with a long calcaneotalotibial nail. Bone Joint J. 2014;96-B(6):817–22. The authors treated 48 frail, geriatric patients who sustained fragility ankle fractures after largely low-energy trauma with a long retrograde hindfoot nail. A return to pre-injury function rate of 90% was reported, as no periprosthetic fractures or nail failure were reported, which the authors at that time attributed to a long nail that bypassed the isthmus of the tibia.
•• Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury. 2017;48(2):519–24. In the only comparison of plate fixation and retrograde hindfoot nailing in the geriatric ankle fracture population, the authors found no functional difference and fewer complications in the hindfoot nail group, suggesting that hindfoot nails can permit a safer and more reliable return to function when performed acutely after an ankle fracture.
Ho B, Ketz J. Primary arthrodesis for tibial pilon fractures. Foot Ankle Clin. 2017;22(1):147–61.
Al-Ashhab M. Primary ankle arthrodesis for severely comminuted tibial pilon fractures. Orthopedics. 2017;40(2):e378–81.
Ochman S, Evers J, Raschke MJ, Vordemvenne T. Retrograde nail for tibiotalocalcaneal arthrodesis as a limb salvage procedure for open distal tibia and talus fractures with severe bone loss. J Foot Ankle Surg. 2012;51(5):675–9. 3 cases, mangled
Hsu AR, Szatkowski JP. Early tibiotalocalcaneal arthrodesis intramedullary nail for treatment of a complex tibial pilon fracture (AO/OTA 43-C). Foot Ankle Spec. 2015;8(3):220–5.
Mohammad HR, A’Court J, Pillai A. Extruded talus treated with reimplantation and primary tibiotalocalcaneal arthrodesis. Ann R Coll Surg Engl. 2017;99(4):e115–7.
Jain NS, Lopez GD, Bederman SS, Wirth GA, Scolaro JA. Surgical management of complex lower-extremity trauma with a long hindfoot fusion nail: a case report. Foot Ankle Spec. 2016;9(4):354–60.
Zelle BA, Gruen GS, McMillen RL, Dahl JD. Primary arthrodesis of the tibiotalar joint in severely comminuted high-energy pilon fractures. J Bone Joint Surg Am. 2014;96(11):e91.
Buckley R, Leighton R, Sanders D, Poon J, Coles CP, Stephen D, et al. Open reduction and internal fixation compared with ORIF and primary subtalar arthrodesis for treatment of Sanders type IV calcaneal fractures: a randomized multicenter trial. J Orthop Trauma. 2014;28(10):577–83.
de Cesar Netto C, Johannesmeyer D, Cone B, Araoye I, Hudson PW, Sahranavard B, et al. Neurovascular structures at risk with curved retrograde TTC fusion nails. Foot Ankle Int. 2017;38(10):1139–45.
Aigner R, Salomia C, Lechler P, Pahl R, Frink M. Relationship of prolonged operative time and comorbidities with complications after geriatric ankle fractures. Foot Ankle Int. 2017;38(1):41–8.
Lee AT, Sundberg EB, Lindsey DP, Harris AH, Chou LB. Biomechanical comparison of blade plate and intramedullary nail fixation for tibiocalcaneal arthrodesis. Foot Ankle Int. 2010;31(2):164–71.
Tarkin IS, Clare MP, Marcantonio A, Pape HC. An update on the management of high-energy pilon fractures. Injury. 2008;39(2):142–54.
Tarkin IS, Mormino MA, Clare MP, Haider H, Walling AK, Sanders RW. Anterior plate supplementation increases ankle arthrodesis construct rigidity. Foot Ankle Int. 2007;28(2):219–23.
Popelka V, Zamborský R. Tibio-calcaneal arthrodesis with vertically placed tricortical bone graft after traumatic talar extrusion—a case report. Acta Chir Orthop Traumatol Cechoslov. 2017;84(6):462–5.
Watanabe K, Teramoto A, Kobayashi T, Ogon I, Sakakibara Y, Kamiya T, et al. Tibiotalocalcaneal arthrodesis using a soft tissue-preserved fibular graft for treatment of large bone defects in the ankle. Foot Ankle Int. 2017;38(6):671–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Both authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Foot and Ankle Trauma
Rights and permissions
About this article
Cite this article
Tarkin, I.S., Fourman, M.S. Retrograde Hindfoot Nailing for Acute Trauma. Curr Rev Musculoskelet Med 11, 439–444 (2018). https://doi.org/10.1007/s12178-018-9507-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-018-9507-y