Abstract
Background
Sepsis-like illness with suspected meningitis or encephalitis is a common reason for using empiric antimicrobial therapy in infants and children. However, in cases of viral meningitis not covered by these antimicrobials, this management is ineffective and due to side effects potentially harmful.
Methods
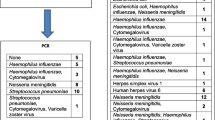
A retrospective analysis of cerebrospinal fluid (CSF) multiplex PCRs (Biofire FilmArray®) in children with clinical suspicion of meningitis, encephalitis or sepsis-like illness was performed over the period of 1 year. Subsequently, a subgroup of children (age of 8–84 days of life) diagnosed with viral meningitis (enterovirus, HHV-6, human parechovirus) was compared to an age-matched control group.
Results
During the study period, the multiplex PCR panel was performed on 187 individual CSF samples that met the inclusion criteria. About half of the patients (92/187) were less than 1 year of age. In 27 cases (14.4%), the PCR yielded a positive result with the majority (12/27) being indicative of an enteroviral infection. In the age group of 8–84 days of life, 36.4% of the patients had a positive result. When the patients with a PCR positive for a viral agent were compared to an age-matched group of patients, no differences were observed regarding symptoms and laboratory parameters. However, the duration of antimicrobial therapy could be significantly reduced through the use of multiplex PCR.
Conclusion
The use of on-site diagnostic multiplex PCR was able to reduce the use of antimicrobials in selected cases. This test can guide clinical decisions earlier during the course of medical care compared to standard diagnostics.


Similar content being viewed by others
References
Aronson PL. Evaluation of the febrile young infant: an update. Pediatr Emerg Med Pract. 2013;10:1–17.
Franco-Paredes C, Lammoglia L, Hernandez I, Santos-Preciado JI. Epidemiology and outcomes of bacterial meningitis in Mexican children: 10-year experience (1993–2003). Int J Infect Dis IJID. 2008;12:380–6.
Ku LC, Boggess KA, Cohen-Wolkowiez M. Bacterial meningitis in infants. Clin Perinatol. 2015;42:29–45 (vii–viii).
Silverman MA, Konnikova L, Gerber JS. Impact of antibiotics on necrotizing enterocolitis and antibiotic-associated diarrhea. Gastroenterol Clin N Am. 2017;46:61–76.
Yamamoto-Hanada K, Yang L, Narita M, Saito H, Ohya Y. Influence of antibiotic use in early childhood on asthma and allergic diseases at age 5. Ann Allergy Asthma Immunol. 2017;119:54–8.
Korpela K, Zijlmans MA, Kuitunen M, Kukkonen K, Savilahti E, Salonen A, de Weerth C, de Vos WM. Childhood BMI in relation to microbiota in infancy and lifetime antibiotic use. Microbiome. 2017;5:26.
Slykerman RF, Thompson J, Waldie KE, Murphy R, Wall C, Mitchell EA. Antibiotics in the first year of life and subsequent neurocognitive outcomes. Acta Paediatr. 2017;106:87–94.
Arora HS, Asmar BI, Salimnia H, Agarwal P, Chawla S, Abdel-Haq N. Enhanced identification of group B Streptococcus and Escherichia Coli in young infants with meningitis using the biofire filmarray meningitis/encephalitis panel. Pediatr Infect Dis J. 2017;36:685–7.
Jorgensen MPHJ, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW. Manual of clinical microbiology. Washington, DC: ASM Press, 2015.
Olijve L, Jennings L, Walls T. Human parechovirus: an increasingly recognized cause of sepsis-like illness in young infants. Clin Microbiol Rev. 2018;31:1–17.
Sharp J, Harrison CJ, Puckett K, Selvaraju SB, Penaranda S, Nix WA, Oberste MS, Selvarangan R. Characteristics of young infants in whom human parechovirus, enterovirus or neither were detected in cerebrospinal fluid during sepsis evaluations. Pediatr Infect Dis J. 2013;32:213–6.
Diaz MG, Garcia RP, Gamero DB, Gonzalez-Tome MI, Romero PC, Ferrer MM, Contreras JR. Lack of accuracy of biomarkers and physical examination to detect bacterial infection in febrile infants. Pediatr Emerg Care. 2016;32:664–8.
Stiemsma LT, Michels KB. The role of the microbiome in the developmental origins of health and disease. Pediatrics. 2018;141:1–22.
Scott FI, Horton DB, Mamtani R, Haynes K, Goldberg DS, Lee DY, Lewis JD. Administration of antibiotics to children before age 2 years increases risk for childhood obesity. Gastroenterology. 2016;151:120–9 e125.
Boussioux C, Rousseau C, Salmona M, Bourdon N, Durand C, Delaire C, Simon F, Gonzalez R, Lallement J, Legoff J. Comparison of FILMARRAY meningitis/encephalitis (ME) panel assay and conventional techniques on the turnaround time of cerebrospinal fluid microbiological testing., ECCMID 2016, 2016.
de Jong EP, van den Beuken MGA, van Elzakker EPM, Wolthers KC, Sprij AJ, Lopriore E, Walther FJ, Brus F. Epidemiology of sepsis-like illness in young infants: major role of enterovirus and human parechovirus. Pediatr Infect Dis J. 2018;37:113–8.
Pons-Salort M, Oberste MS, Pallansch MA, Abedi GR, Takahashi S, Grenfell BT, Grassly NC. The seasonality of nonpolio enteroviruses in the United States: patterns and drivers. Proc Natl Acad Sci USA. 2018;115:3078–83.
Teoh HL, Mohammad SS, Britton PN, Kandula T, Lorentzos MS, Booy R, Jones CA, Rawlinson W, Ramachandran V, Rodriguez ML, et al. Clinical characteristics and functional motor outcomes of enterovirus 71 neurological disease in children. JAMA Neurol. 2016;73:300–7.
Hixon AM, Clarke P, Tyler KL. Evaluating treatment efficacy in a mouse model of enterovirus D68-associated paralytic myelitis. J Infect Dis. 2017;216:1245–53.
Bissel SJ, Auer RN, Chiang CH, Kofler J, Murdoch GH, Nix WA, Painter M, Richer M, Sartelet H, Wang G, et al. Human parechovirus 3 meningitis and fatal leukoencephalopathy. J Neuropathol Exp Neurol. 2015;74:767–77.
Britton PN, Dale RC, Nissen MD, Crawford N, Elliott E, Macartney K, Khandaker G, Booy R, Jones CA. Parechovirus encephalitis and neurodevelopmental outcomes. Pediatrics. 2016;137:e20152848.
Wildenbeest JG, Wolthers KC, Straver B, Pajkrt D. Successful IVIG treatment of human parechovirus-associated dilated cardiomyopathy in an infant. Pediatrics. 2013;132:e243–7.
Green DA, Pereira M, Miko B, Radmard S, Whittier S, Thakur K. Clinical significance of human herpesvirus 6 positivity on the FilmArray meningitis/encephalitis multiplex PCR panel. Clin Infect Dis. 2018. https://doi.org/10.1093/cid/ciy288.
Asano Y, Yoshikawa T, Suga S, Kobayashi I, Nakashima T, Yazaki T, Kajita Y, Ozaki T. Clinical features of infants with primary human herpesvirus 6 infection (exanthem subitum, roseola infantum). Pediatrics. 1994;93:104–8.
Zhang E, Bell AJ, Wilkie GS, Suarez NM, Batini C, Veal CD, Armendariz-Castillo I, Neumann R, Cotton VE, Huang Y, et al. Inherited chromosomally integrated human herpesvirus 6 genomes are ancient, intact, and potentially able to reactivate from telomeres. J Virol. 2017;91:1–19.
Caserta MT, Hall CB, Schnabel K, McIntyre K, Long C, Costanzo M, Dewhurst S, Insel R, Epstein LG. Neuroinvasion and persistence of human herpesvirus 6 in children. J Infect Dis. 1994;170:1586–9.
Basmaci R, Mariani P, Delacroix G, Azib S, Faye A, Taha MK, Bingen E, Bonacorsi S, Romero JR, Rotbart HA, et al. Enteroviral meningitis does not exclude concurrent bacterial meningitis. J Clin Microbiol. 2011;49:3442–3.
Piccirilli G, Chiereghin A, Gabrielli L, Giannella M, Squarzoni D, Turello G, Felici S, Vocale C, Zuntini R, Gibertoni D, et al. Infectious meningitis/encephalitis: evaluation of a rapid and fully automated multiplex PCR in the microbiological diagnostic workup. New Microbiol. 2018;41:118–25.
Naccache SN, Lustestica M, Fahit M, Mestas J, Bard JD. One year in the life of a rapid syndromic panel for meningitis/encephalitis: a pediatric tertiary care facility’s experience. J Clin Microbiol. 2018;56:1–11.
Dien Bard J, Alby K. Point-counterpoint: meningitis/encephalitis syndromic testing in the clinical laboratory. J Clin Microbiol. 2018;56:1–10.
Rossi AF, Khan D. Point of care testing: improving pediatric outcomes. Clin Biochem. 2004;37:456–61.
Ferreira CES, Guerra JCC, Slhessarenko N, Scartezini M, Franca CN, Colombini MP, Berlitz F, Machado AMO, Campana GA, Faulhaber ACL, et al. Point-of-care testing: general aspects. Clin Lab. 2018;64:1–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JH has received speaker fees and MMB has been invited to a seminar by BioMerieux, and the other authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Eichinger, A., Hagen, A., Meyer-Bühn, M. et al. Clinical benefits of introducing real-time multiplex PCR for cerebrospinal fluid as routine diagnostic at a tertiary care pediatric center. Infection 47, 51–58 (2019). https://doi.org/10.1007/s15010-018-1212-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1212-7