Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1666
Peer-review started: June 24, 2014
First decision: August 6, 2014
Revised: August 22, 2014
Accepted: September 30, 2014
Article in press: September 30, 2014
Published online: February 7, 2015
Bleeding of peptic ulcer at the posterior duodenal bulb still is a particular endoscopic challenge with increased risk of treatment failure and worse outcome. In this article, we report successful treatment of an actively bleeding peptic ulcer located at the posterior duodenal wall, using an over-the-scope-clip in the case of a 54-year-old male patient with hemorrhagic shock. Incident primary hemostasis was achieved and no adverse events occurred during a follow-up of 60 d.
Core tip: Bleeding of peptic ulcer at the posterior duodenal bulb still is a particular endoscopic challenge with increased risk of treatment failure and worse outcome. In this article, we report successful treatment of an actively bleeding peptic ulcer located at the posterior duodenal wall, using an over-the-scope-clip in the case of a 54-year-old male patient with hemorrhagic shock. Incident primary hemostasis was achieved and no adverse events occurred during a follow-up of 60 d.
- Citation: Brechmann T, Schmiegel W. Successful treatment of life-threatening bleeding from a duodenal posterior bulb peptic ulcer by an over-the-scope-clip. World J Gastroenterol 2015; 21(5): 1666-1669
- URL: https://www.wjgnet.com/1007-9327/full/v21/i5/1666.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i5.1666
Acute upper gastrointestinal (GI) bleeding represents a major, potentially life-threatening complication of gastroduodenal ulcer disease with high morbidity. Especially localization on the posterior wall of the duodenal bulb has been proven to be risk factor of adverse outcome in bleeding peptic ulcers[1] and predictor of treatment-failure[2]. In retrospective analysis, rebleeding, despite high rate of successful initial hemostasis, frequently occurs in actively bleeding peptic ulcers: i.e., 20% in Ia of Forrest-classification and about 27% in Ib[3]. In that particular study, the higher rate of rebleeding in oozing rather than in spurting lesions might be explained by more frequent use of monotherapy (64.5% for Ia vs 87.8% for Ib); in older prospective studies, patients with spurting arterial bleeding required more clips compared to patients with oozing ones and showed lower rates of hemostasis[4,5]. Since then, endoscopic treatment has advanced significantly, but the success rate of endoscopic hemostasis and the rate of rebleeding have scarcely been reported. The full wall grabbing over-the-scope-clip (OTSC) that was recently developed by Ovesco (Ovesco Endoscopy AG, Dorfackerstr. 26, 72074 Tübingen, Germany), has been approved not only for closing perforations, but also for the treatment of bleeding. While most case studies describe closure of perforation, only few reports, however, claim efficacy of OTSC in treatment of severe peptic ulcerous bleeding. In literature, most cases, in which an OTSC was applied, deal with iatrogenic lesions, while only a small number of series with few cases describe hemostasis of upper GI-bleeding[6-10]. Nevertheless, only one case deals with severe duodenal bleeding[8].
A 54-year-old male patient came to our hospital with hematemesis. He reported that he had had recurrent gastric and duodenal ulcers 30 to 40 years ago during the second decade of life, which were back then diagnosed by radiological means. No comorbidity was known; the patient was neither on non-steroidal anti-inflammatory drugs nor on any other medication. He exhibited signs of hypovolemic shock (heart rate 130 bpm, blood pressure 100/55 mmHg); digitorectal examination disclosed melena; further physical examination revealed no pathological findings.
Red blood cell count (RBC) was determined 5.6 g/dL, while the other laboratory tests were within normal range.
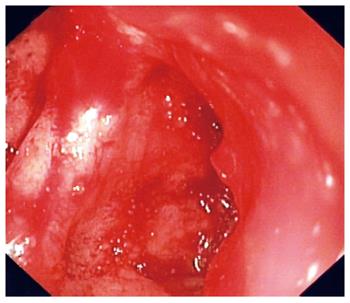
Cardiocirculatory stabilization was achieved by transfusion of four units of erythrocyte concentrates, one unit of fresh frozen plasma and crystalloid infusion. Immediate medication with double standard dose of proton pump inhibitor (pantoprazole 80 mg) intravenously, followed by constant infusion (pantoprazole 8 mg/h) were administered, and we performed an emergent esophagogastroduodenoscopy (EGD). Besides a coagulum in the fundus, endoscopy with a therapeutic endoscope (Olympus 160-XTQ) revealed an ulcer on the distal posterior wall of the bulb with severe spurting bleeding (Figure 1). Conventional clipping did not seem promising due to the tangential position of the bleeding vessel. Furthermore, limited space and severe bleeding inhibited targeting HemoSpray® (Cook Medical, Bloomington, IN 47402-4195, United States) optimally, which resulted in a clot in the lumen, but not on the bleeding source.
Thus, we decided to apply an OTSC. Consequently, the scope was replaced by a therapeutic endoscope with smaller diameter (Olympus 160-TQ) and we attached a type gc OTSC with 6 mm of cap depth to the instrument. This version of the clip allows optimal grip of the “bear-claw” on the taut tissue of the posterior bulb.
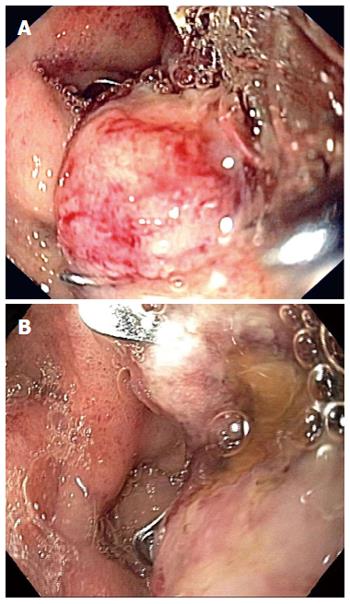
After applying anaesthetic gel on the device, the scope could be inserted easily. In the course of the procedure, we redisplayed and catched the lesion with the OTSC Anchor (OTSC, Ovesco, 72074 Tübingen, Germany). By sucking the duodenal wall and pulling the anchor, it was then possible to place enough tissue within the cap so that the OTSC could finally be applied to the lesion. The bleeding stopped instantly (Figure 2A).
In the course of hospitalization, RBC remained stable and finally increased without further transfusion. As the patient suffered from iron-deficiency (decreased Ferritin-level), we administered iron intravenously in the form of carboxymaltose. Both, pathohistological evaluation and urease test showed that Helicobacter pylori was the cause for the patient’s ulcer disease. Treatment with clarithromycin 500 mg b.i.d. and amoxicillin 1000 mg b.i.d. was introduced. Demission was possible within one week after the emergent EGD had been performed. Once the patient had been stabilized and proven fit for examination, a subsequent EGD showed that the edema was diminishing in size; the scope could pass the lesion freely (Figure 2B); red blood cell count was 8.6 g/dL. Until the visit 30 d after intervention, the erythrocytes had increased up to a level of 9.9 g/dL. No adverse events were reported during a follow-up of 60 d.
This case, to our knowledge, represents the second case of treatment of a peptic ulcer with spurting bleeding applying OTSC and the first treatment ever on primary instance right after failure of HemoSpray®. Besides closure of perforations, retrospective case-series to date report, the treatment of bleeding-sources in the stomach or colorectum, and predominantly iatrogenic lesions. In theory, there are four major challenges that make using an OTSC difficult: (1) the tight tissue; (2) the limited cavity of the duodenum; and (3) the thin wall and the fact that the area is hard to reach. Theoretically, adverse events like perforation, misplacement or treatment failure and even subsequent duodenal stenosis are possible. This proves the interestingness of our case, as it does not only emphasize the usefulness, but also the safety of the “bear-claw” in treating severe, life-threatening bleeding during emergency endoscopy, even in a challenging localization of posterior bulb. We suggest to conduct prospective studies in order to prove OTSC as the device of choice.
The authors would like to thank Daniel-Theo Brechmann for linguistic revision.
A middle-aged male patient presented with hemorrhagic shock and signs of gastrointestinal bleeding.
The bleeding source was a duodenal ulcer Forrest Ia.
Different bleeding sources especially of the upper gastrointestinal tract have to taken into account.
Red blood cell count was as low as 5.6 g/dL.
Emergent endoscopy showed a spurting bleeding ulcer at the posterior wall of the duodenal bulb.
Histopathological examination showed Gastritis due to Helicobacter pylori.
Endoscopic treatment included hemospray and an over-the-scope-clip (OTSC), medical treatment included PPI-therapy and an antiobiotic regimen.
Several case report showed the potential role of the OTSC in other localisations, i.e., stomach and colon.
The OTSC is a device that allows endoscopic full wall closure for cases of perforations or bleeding.
The OTSC offers a promising opportunity in an difficult-to-reach and difficult-to-treat localisation of severe ulcerous bleeding and can be placed without downsides.
This report is very interesting and well illustrated about the utility of this form of endoscopic therapy in difficult ulcer bleeding control such are the posterior will placed.
P- Reviewer: Nakajima N, Perathoner A, Rodrigo L, Slomiany BL S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
| 1. | Kolkman JJ, Meuwissen SG. A review on treatment of bleeding peptic ulcer: a collaborative task of gastroenterologist and surgeon. Scand J Gastroenterol Suppl. 1996;218:16-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Choudari CP, Rajgopal C, Elton RA, Palmer KR. Failures of endoscopic therapy for bleeding peptic ulcer: an analysis of risk factors. Am J Gastroenterol. 1994;89:1968-1972. [PubMed] [Cited in This Article: ] |
| 3. | Endo M, Higuchi M, Chiba T, Suzuki K, Inoue Y. Present state of endoscopic hemostasis for nonvariceal upper gastrointestinal bleeding. Dig Endosc. 2010;22 Suppl 1:S31-S34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Raju GS, Gajula L. Endoclips for GI endoscopy. Gastrointest Endosc. 2004;59:267-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 142] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 5. | Lai YC, Yang SS, Wu CH, Chen TK. Endoscopic hemoclip treatment for bleeding peptic ulcer. World J Gastroenterol. 2000;6:53-56. [PubMed] [Cited in This Article: ] |
| 6. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-2760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 101] [Cited by in F6Publishing: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162-3164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 8. | Mönkemüller K, Toshniwal J, Zabielski M, Vormbrock K, Neumann H. Utility of the “bear claw”, or over-the-scope clip (OTSC) system, to provide endoscopic hemostasis for bleeding posterior duodenal ulcers. Endoscopy. 2012;44 Suppl 2 UCTN:E412-E413. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Repici A, Arezzo A, De Caro G, Morino M, Pagano N, Rando G, Romeo F, Del Conte G, Danese S, Malesci A. Clinical experience with a new endoscopic over-the-scope clip system for use in the GI tract. Dig Liver Dis. 2009;41:406-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-167. [PubMed] [Cited in This Article: ] |