Abstract
The relationship between gut microbiota and the host is symbiotic and mutualistic. Gut microbiota has been shown to influence many aspects of host biology, including metabolism, development, and immunity. Due to the close proximity of the microbes to epithelial surfaces, this barrier represents the primary gateway for potential interactions. Alterations in the balance between gut microbiota and host are now clearly recognized as an influencing factor in the cause of a wide range of intestinal diseases. It is therefore important to gain a better understanding of the mechanisms regulating signals that gut microbiota provides to intestinal epithelial cells. In this context, it is expected that an important role is to be played by intestinal stem cells in their role in epithelial regeneration, homeostasis post-damage repair.
Similar content being viewed by others
Introduction
The gastrointestinal tract is populated by a diverse community of microorganisms, mainly dominated by bacteria, but also comprised of archaea, fungi, protozoa, and viruses. Collectively, these populations are considered the gut microbiota. The microbiota has been defined as a “forgotten organ” [1], playing a central role in health and disease. The microbiota provides protective functions by forming a natural defense barrier. It has metabolic functions such as the fermentation of non-digestible dietary residues, the synthesis of vitamins, and the detoxification of dietary carcinogens. Moreover, the gut microbiota interacts with the immune system, stimulating its development and maturation [2].
The microbiota, as well as bacterial products and bacterial metabolites, provide continuous stimuli to the entire epithelial layer, possibly indirectly affecting stem cells that could sense signals from neighboring cells responding to bacterial agonists. These signals could influence the survival of stem cells and therefore control both proliferation and regeneration of the whole epithelium.
Microbiota is recognized by the host through pattern recognition receptors (PRRs). Toll-like receptors (TLRs) and nucleotide-binding oligomerization domains (NODs) are the main receptors involved in the recognition of conserved bacterial motifs defined as “microbe-associated molecular patterns” (MAMPs) [3]. TLRs are transmembrane proteins located at the cellular plasma membrane or at the endosomal membranes. Instead, the NODs are cytosolic proteins. PRRs are expressed by both immune and non-immune cells, playing a major role in response to specific MAMPs, especially those from pathogens in order to activate the host immune response. Indeed, in the gut, PRRs seem to be crucial for bacterial-host communications and for maintaining intestinal homeostasis [4]. One can reasonably hypothesize that stem cells could also express PRRs to recognize bacteria, therefore directly responding themselves to the microbiota.
Lesson from Germ Free Animals
Comparisons of germ free (GF) and conventionally raised animals have demonstrated the main role of the gut microbiota on homeostasis not only at the mucosal level, but also at the systemic level. Moreover, using mono- or poly-associated animals with different bacterial species or animals treated with particular microbial motifs has allowed the identification of specific microbe-host interaction pathways contributing to a healthy state.
For instance, GF animals show an altered rate of epithelial proliferation. GF rats have a slight hyperplasia of their intestinal villi, which is associated with a comparatively short cell cycle time. Similarly, in the colon of GF or antibiotic-treated mice, the cell proliferation rate is reduced and their crypts contain fewer cells than those of conventional mice [5, 6]. Several other alterations have been shown in the gut of GF animals, such as reduction of the villous capillary network, a reduction in digestive enzymes activity, the presence of smaller Peyer’s patches, and impairment in the gut peristaltic activity [1].
Conversely, the colonization of GF mice with bacteria often restores the above-mentioned parameters to levels similar to those of conventionally raised mice. For instance, mice mono-colonized with Bacteroides thetaiotaomicron present an alteration in the expression of genes influencing mucosal barrier functions, nutrient absorption, metabolism, angiogenesis, and development of the enteric nervous system [7, 8]. Alengath et al. have shown that the epigenome-modifying enzyme histone deacetylase 3 (HDAC3) has a central role in maintaining intestinal homeostasis, especially following damage and inflammation. Intestinal epithelial cell proliferation, epithelial barrier function, and Paneth cell number were all altered in mice lacking HDAC3 in epithelial cells [9]. These parameters nearly returned to normal when animals were raised in GF conditions, showing that the presence of commensal bacteria facilitates the expression of networks of genes that regulate epithelial function and tissue homeostasis. The microbiota is also necessary to stimulate the development of the host immune system. Several studies have shown that bacteria or bacterial motifs are necessary for proper host development not only of the gut but also, for instance, of the immune system. A first example was provided by Mazmanian et al. [10]. GF animals show a lower proportion of CD4+ T-cell compared to conventionally raised mice. The colonization of GF mice with Bacteroides fragilis, producing polysaccharide A (PSA), or purified PSA alone was sufficient to expand T-cell populations. The Eberl group has shown that fragments of peptidoglycan released by gram-negative bacteria are necessary and sufficient to induce the genesis of isolated lymphoid follicles [11]. Interestingly, the same bacterial products, released by Vibrio fischeri, have been shown to be essential in the development of the light-emitting organ in the squid [12]. This highlights the fact that the conserved bacterial motifs can stimulate different organs in different species, but are still necessary for the full development of the host.
Not only bacterial motifs, but also bacterial metabolites influence host homeostasis. For example, the fermentation of carbohydrates by the microbiota produces short chain fatty acids (SCFAs), such as butyrate and propionate, that provide an important source of nutrients for the epithelium, but also act as signaling molecules. Recently, several SCFA receptors have been identified [13], increasing the number of potential pathways regulated by these products, including lipid and glucose metabolism, proliferation, and differentiation [14]. The G-protein-coupled receptor GPR43, which is highly expressed in neutrophils and eosinophils, has been found to recognize the SCFAs, establishing a link between these compounds and the regulation of immune and inflammatory responses [15].
Microbiota and Intestinal Homeostasis
Drosophila has provided an important model to study interactions of microbiota with stem cells. As in mammals, Drosophila intestinal stem cells have the properties to self-regenerate and provide enteroblasts (corresponding to transit amplifying cells in mammals) that then differentiate in enterocytes and enteroendocrine cells [16]. In the recent years, several studies have highlighted how the microbiota impacts both gut immunity and also intestinal tissue homeostasis. In 2009, several studies reported how proliferation of intestinal stem cells in the Drosophila midgut is activated in response to both infectious and indigenous bacteria. In steady-state conditions, as well as following damage or bacterial infection, enterocytes produce cytokines which activate the JAK-STAT (Janus kinase–signal transducers and activators of transcription) pathway in stem cells, thereby promoting proliferation [17, 18]. More recently, Jones et al. showed that the microbiota could stimulate oxidative stress responses and particularly Nox1 (NADPH oxidase 1)-dependent ROS generation, consequently increasing cell proliferation in intestinal stem cells [19].
In 2012, our group identified the presence of a so called “crypt-specific core microbiota” (CSCM) in both the ceacal and colonic crypts of mice [20•]. Using laser capture microdissection (LCM), pyrosequencing, and FISH, the dominant species present in the colonic crypts were identified as being aerobic, non-fermenting bacteria belonging primarily to the genus Acinetobacter. The presence of bacteria in the crypt had been shown in patients suffering from ulcerative colitis [21]. However, in this study, we were able to demonstrate the presence of bacteria in the colonic crypts of healthy animals, identifying a specific core microbiota. These results suggest that particular species may have been evolutionarily selected because they provide a specific advantage to the host, probably having particular MAMPs or producing specific metabolites that maintain crypt homeostasis, potentially directly acting on stem cells.
In 2004, Rakoff-Nahoum et al. showed the crucial role played by TLRs in intestinal homeostasis [22]. Comparing MyD88 KO mice or TLR2 and/or TLR4 KO mice to wt mice, they showed that the activation of TLRs by the commensal microbiota is critical for protection against injury, such as DSS-induced damage. This was the first evidence of the effect of the microbiota, particularly the released-MAMPs, in preserving gut homeostasis and promoting tissue repair and host survival upon recognition of bacterial products through PRRs.
Microbiota and Intestinal Stem Cells
The epithelial lining is designed to carry out several functions, including digestion, absorption of the nutrients, and protection from pathogens or chemicals in transit in the lumen. Cells naturally die, though pathogens and toxins may accelerate the death rates, thus revealing a need for physiological regeneration and its acceleration to compensate for injury. The intestinal epithelium is the most vigorously self-renewing tissue among adult mammals thanks to the high activity of intestinal stem cells. After division, stem cells produce highly proliferative progenitors, known as transit amplifying (TA) cells. TA cells divide 2–3 times and following a gradient of factors present along the crypt epithelium, differentiate into absorptive or secretory lineages while migrating upwards. In the small intestine, those cells reach the top of the villi in 3–5 days. The only cells escaping the ascent flow are Paneth cells. These cells originate from dedicated secretory progenitors located at the base of the TA compartment and are subjected to downward migration to the bottom of the crypt where they can persist for 1 month or more [23••]. Stem cells are located at the base of intestinal crypts. There the Wnt pathway provides a proper niche to maintain their “stemness”, meaning the properties of self-renewal and differentiation. The main player in the canonical Wnt-pathway is β-catenin. In the presence of a Wnt signal, β-catenin translocates into the nucleus and binds to transcription factors of the T cell factor/lymphocyte enhancer factor (TCF/LEF) family. This active complex allows transcription of target genes supporting the proliferation program. Instead, in the absence of a Wnt signal, β-catenin is phosphorylated and degraded by the proteasome. This represents a signal to block proliferation and to begin the differentiation step for which the Notch pathway plays a major role in subsequent cell fate decisions. The Wnt and Notch ligands are secreted by the epithelium and the underlying mesenchymal cells, thereby providing a proper niche at the bottom of the crypt for the stem cells and, conversely, inducing cell differentiation outside the crypt [23••].
Based on the importance of the Wnt-pathway to maintain “stemness”, Clevers’ group studied the intestinal Wnt target genes specifically expressed in the crypt in order to identify specific stem cell genes. From this panel, the lgr5 gene was identified as a Wnt target selectively expressed at the bottom of adult intestinal crypts. Lgr5 is an orphan receptor of the G-protein coupled receptor (GPCR) superfamily [24]. Recently, R-spondins were identified as the ligands for Lgr5-receptors, the recognition of these molecules enhancing Wnt signaling [25]. The cells expressing Lgr5 correspond to the crypt base columnar (CBC) cells located at the base of crypts and intercalated with Paneth cells. Already in 1974, Cheng and Leblond proposed that these cells possessed multipotential capacities, being able to generate different epithelial lineages [26]. More direct evidence to the fact that Lgr5-expressing CBC cells are bona fide intestinal stem cells was provided by Clevers’ group using in vivo lineage tracing experiments and ex vivo assays. They showed that when sorted and cultivated in Matrigel with a cocktail of growth factors, Lgr5+ cells give rise to three-dimensional structures defined as mini-guts or organoids [27]. These structures mimic the epithelial architecture observed in vivo, with crypt- and villus-like domains. They harbor the four common lineages (e.g., enterocytes, enteroendocrine cells, goblet cells, and Paneth cells) and also stem cells located at the level of budding structures, corresponding to neocrypts.
Until now, it has been difficult to describe direct interactions of bacteria with intestinal stem cells due to the lack of specific markers for these populations. Therefore, only putative stem cells were analyzed. Following the identification of Lgr5 as a marker for the CBC stem cells, researchers have begun to evaluate the direct effect of bacteria on intestinal stem cells.
It has been shown by Neal et al. that in intestinal tissue, TLR4 is mainly expressed at the bottom of the crypts, in particular, that Lgr5+ intestinal stem cells express this receptor [28••]. Using the organoid model, they showed that in the presence of LPS, the rate of cellular apoptosis increased, and concomitantly, the rate of epithelial proliferation decreased. To further demonstrate the TLR4-mediated effect of LPS on intestinal stem cells, they generated mice in which TLR4 was selectively deleted in Lgr5+ stem cells. The engineered mice presented a mosaic pattern of TLR4 deletion, with some crypts expressing TLR4 and some not. This model allowed the comparison of TLR4-expressing and TLR4-deficient crypts within the same animal under the same conditions. Upon injection of LPS in the animals, they demonstrated a reduction in proliferation and an increase in apoptosis only in the crypts expressing TLR4, independent of TNF signals from other cell types. Moreover, they showed that the apoptotic signal was dependent on up-regulation of PUMA through TRIF in a MyD88- and TNF-independent manner. In another study using a mouse model over-expressing TLR4 in the intestinal epithelium (villin-TLR4 mice), the opposite effect was observed [29••]. The presence of TLR4 was linked to increased proliferation and expansion of Lgr5+ cells. This was due to the activation of the Wnt/β-catenin pathway through TLR4. The two experimental models are quite different, and this could explain the observed discrepancies. In the first model, animals were injected with LPS that provides a boost to the host-response. Conversely, in the second study, animals were not stimulated with exogenous LPS, thus remaining at homeostatic levels of MAMPs but rather over-expressing the receptor. Further experiments are thus necessary to better understand the role of TLR4 in intestinal stem cells.
In the context of examining the crypt-microbiota interface, our own group evaluated the potential influence of bacterial products on organoid growth [30••]. We found that the muramyl-dipeptide (MDP), a component of peptidoglycan, was inducing higher yields of organoids in a Nod2-dependent manner, providing an indication that MDP protects stem cells from stress induced by the extraction protocol. Using co-culture of single intestinal stem cells and Paneth cells from wt and/or NOD2KO mice, we demonstrated that this effect was due to the expression of Nod2 in stem cells and not in Paneth cells. To better evaluate the cytoprotective effect of MDP on the stem cells, we first performed in vivo experiments on mice in which the microflora was depleted by antibiotic treatment. We showed that mice gavaged with MDP were protected from the effects of doxorubicin, a DNA-intercalating agent that induces high levels of oxidative stress. To test the existence of a NOD2-dependent pathway of stem cell cytoprotection in the presence of microbiota-produced MDP, we carried out similar experiments in conventional wt and NOD2KO mice. We observed that wt mice, not NOD2KO mice, were able to regenerate the gut upon treatment with doxorubicin. Moreover, the wt mice presented higher numbers of crypt survival compared to NOD2KO mice, indicating a protective effect of NOD2. We also showed that crypts extracted from doxorubicin-treated mice were much more responsive to MDP regarding the yields of organoids. Therefore, in the presence of stress, such as doxorubicin, the stem cells are more prone to respond to the MDP released by the microflora that enhances their protection from injury. This work highlighted a new role for NOD2 in intestinal homeostasis. In a steady-state condition, the bacteria perhaps do not give any specific advantage to stem cells, as indicated by the fact that NOD2KO mice are viable and do not present any particular difference compare to wt mice. However, upon injury, the presence of the microbiota, particularly the released MDP, has a protective effect on stem cells, making them more reactive to MDP itself and more resistant to death.
Conclusions
The role of gut microbiota in protecting the host from potential harm from chemicals or pathogens is crucial. This is due not only to the presence of the bacteria over the epithelial layer, providing a physical barrier to protect against various types of luminal insults, but also their communicative cross-talks with host cells. Through direct contact or release of products and/or metabolites, the bacteria modulate gut homeostasis, regulating for instance regeneration, repair, and differentiation.
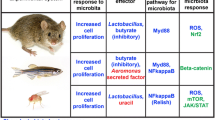
It was to be expected that considering their crucial role in the latter process, stem cells might emerge as major partners in the microbe-host cross-talks. The recent discovery of specific intestinal stem cells markers has opened a new field of study evaluating to which extent the microbiota could directly cross-talk with stem cells. Recent evidences highlighting the expression and activity of PRRs, such as TLR4 and NOD2, suggest direct implications of bacterial products on the survival of stem cells. The two contributions are actually proposing two opposite effects. On one side, LPS provides a death signal, while MDP provides a cytoprotective signal (Fig 1).
Balance of MAMPs in the crypts. It has been reported that Lgr5+ intestinal stem cells could sense Lipopolysaccharide (LPS) and muramyl-dipeptide (MDP) through TLR4 and NOD2, respectively (see text). The two bacterial products induce opposite effects on the stem cells: apoptosis versus survival. Possibly, in the crypts, there is a balance between the signals that provide a homeostatic equilibrium
This discrepancy could be explained by the fact that in the gut, both products are present though at different concentrations. The two signals may somewhat annihilate each other in function of their respective concentration. Also, endotoxins are known to vary in toxicity depending on their acylation and phosphorylation; these modifications vary and are determined by their species of origin, leading to variations in host recognition. Moreover, although the MAMPs are conserved motifs, different bacteria can present modified structures, such as the LPS, or have a different shedding of these molecules and this could alter the host response. It is also important to take into consideration that in vivo stem cells are not isolated but they are in a niche that provides stimuli to them. Within this context, the response of all cells present in this context should be considered, including those of the immune system.
The interaction between microbiota and intestinal stem cells is a new and promising field that could contribute to a better understanding of the physiology of the gut as well as diseases, such as the inflammatory bowel diseases.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
O’Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep. 2006;7:688–93.
Chow J, Lee SM, Shen Y, et al. Host-bacterial symbiosis in health and disease. Adv Immunol. 2010;107:243–74.
Kawai T, Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011;34:637–50.
Abreu MT, Fukata M, Arditi M. TLR signaling in the gut in health and disease. J Immunol. 2005;174:4453–60.
Alam M, Midtvedt T, Uribe A. Differential cell kinetics in the ileum and colon of germfree rats. Scand J Gastroenterol. 1994;29:445–51.
Reikvam DH, Erofeev A, Sandvik A, et al. Depletion of murine intestinal microbiota: Effects on gut mucosa and epithelial gene expression. PLoS One. 2011;6:e17996. Public Library of Science.
Zocco MA, Ainora ME, Gasbarrini G, et al. Bacteroides thetaiotaomicron in the gut: Molecular aspects of their interaction. Dig Liver Dis. 2007;39:707–12.
Stappenbeck TS, Hooper LV, Gordon JI. Developmental regulation of intestinal angiogenesis by indigenous microbes via Paneth cells. Proc Natl Acad Sci U S A. 2002;99:15451–5.
Alenghat T, Osborne LC, Saenz SA, et al. Histone deacetylase 3 coordinates commensal-bacteria-dependent intestinal homeostasis. Nature. 2013;504:153–7.
Mazmanian SK, Liu CH, Tzianabos AO, et al. An immunomodulatory molecule of symbiotic bacteria directs maturation of the host immune system. Cell. 2005;122:107–18.
Bouskra D, Brézillon C, Bérard M, et al. Lymphoid tissue genesis induced by commensals through NOD1 regulates intestinal homeostasis. Nature. 2008;456:507–10.
Koropatnick TA, Engle JT, Apicella MA, et al. Microbial factor-mediated development in a host-bacterial mutualism. Science. 2004;306:1186–8.
den Besten G, van Eunen K, Groen AK, et al. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54:2325–40.
Guzman JR, Conlin VS, Jobin C. Diet, microbiome, and the intestinal epithelium: an essential triumvirate? Biomed Res Int. 2013;2013:425146.
Maslowski KM, Vieira AT, Ng A, et al. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature. 2009;461:1282–6.
Micchelli CA, Perrimon N. Evidence that stem cells reside in the adult Drosophila midgut epithelium. Nature. 2006;439:475–9.
Buchon N, Broderick NA, Chakrabarti S, et al. Invasive and indigenous microbiota impact intestinal stem cell activity through multiple pathways in Drosophila. Genes Dev. 2009;23:2333–44.
Jiang H, Patel PH, Kohlmaier A, et al. Cytokine/Jak/Stat signaling mediates regeneration and homeostasis in the Drosophila midgut. Cell. 2009;137:1343–55.
Jones RM, Luo L, Ardita CS, et al. Symbiotic lactobacilli stimulate gut epithelial proliferation via Nox-mediated generation of reactive oxygen species. EMBO J Nat Publ Group; 2013;32:3017–28.
Pedron T, Mulet C, Dauga C, et al. A crypt-specific core microbiota resides in the mouse colon. mBio. 2012;3:e00116–12. This paper provides the evidence that the murin colonic crypts are occupied by defined bacterial species.
Sokol H, Vasquez N, Hoyeau-Idrissi N, et al. Crypt abscess-associated microbiota in inflammatory bowel disease and acute self-limited colitis. World J Gastroenterol. 2010;16:583–7.
Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, et al. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–41.
Barker N. Adult intestinal stem cells: Critical drivers of epithelial homeostasis and regeneration. Nat Rev Mol Cell Biol. 2014;15:19–33. Review describing the current models of stem cell-driven epithelial homeostasis and repair in the intestine.
Barker N, van Es JH, Kuipers J, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–7.
de Lau W, Barker N, Low TY, et al. Lgr5 homologues associate with Wnt receptors and mediate R-spondin signalling. Nature. 2011;476:293–7.
Cheng H, Leblond CP. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine V. Unitarian Theory of the origin of the four epithelial cell types. Am J Anat. 1974;141:537–61.
Sato T, Vries RG, Snippert HJ, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–5.
Neal MD, Sodhi CP, Jia H, Dyer M, Egan CE, Yazji I, et al. Toll-like receptor 4 is expressed on intestinal stem cells and regulates their proliferation and apoptosis via the p53 up-regulated modulator of apoptosis. J Biol Chem. 2012;287:37296–308. TLR4 is expressed in stem cells where it contributes to regulate their proliferation and apoptosis through activation of PUMA.
Santaolalla R, Sussman DA, Ruiz JR, et al. TLR4 activates the β-catenin pathway to cause intestinal neoplasia. PLoS ONE Public Libr Sci. 2013;8:e63298. The over-expression of TLR4 in the gut increases stem cell population in the gut and induces a higher rate of epithelial proliferation.
Nigro G, Rossi R, Commere P-H, et al. The cytosolic bacterial peptidoglycan sensor Nod2 affords stem cell protection and links microbes to gut epithelial regeneration. Cell Host Microbe. 2014;15:792–8. NOD2 expressed in the stem cells links the microbes and tissue regeneration.
Compliance with Ethics Guidelines
Conflict of Interest
Giulia Nigro and Philippe J. Sansonetti declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Microbiome and Stem Cell Function
Rights and permissions
About this article
Cite this article
Nigro, G., Sansonetti, P.J. Microbiota and Gut Stem Cells Cross-Talks: A New View of Epithelial Homeostasis. Curr Stem Cell Rep 1, 48–52 (2015). https://doi.org/10.1007/s40778-014-0005-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40778-014-0005-x