Key Points
-
Ureteral stents are associated with complications including infection, encrustation, haematuria and discomfort that can be caused by tissue irritation
-
The role of bacterial adhesion and biofilm formation on stents in stent-associated UTIs is unclear and development of UTIs and their treatment might depend on patient immune status
-
Encrustation and calcification are common problems that can lead to severe complications, which can be prevented by implementing electronic systems to monitor stent dwell times
-
Metal stents are a good alternative to polymer stents in the treatment of extrinsically caused ureteral obstruction; flexible and drug-eluting metal designs could help ameliorate discomfort and stenosis, respectively
-
Biodegradable ureteral stents could avoid complications, such as encrustation, but flaws in their biocompatibility still need to be addressed
-
Future stent design will focus on biodegradable and metal stents that elute drugs to prevent complications and are engineered to treat specific urological conditions
Abstract
Ureteral stents are one of the most commonly used devices in the treatment of benign and malignant urological diseases. However, they are associated with common complications including encrustation, infection, pain and discomfort caused by ureteral tissue irritation and possibly irregular peristalsis. In addition, stent migration and failure due to external compression by malignancies or restenosis occur, albeit less frequently. As these complications restrict optimal stent function, including maintenance of adequate urine drainage and alleviation of hydronephrosis, novel stent materials and designs are required. In recent years, progress has been made in the development of drug-eluting expandable metal stents and biodegradable stents. New engineering technologies are being investigated to provide stents with increased biocompatibility, decreased susceptibility to encrustation and improved drug-elution characteristics. These novel stent characteristics might help eliminate some of the common complications associated with ureteral stenting and will be an important step towards understanding the behaviour of stents within the urinary tract.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Finney, R. P. Experience with new double J ureteral catheter stent. J. Urol. 120, 678–681 (1978).
Joshi, H. B. et al. Ureteral stent symptom questionnaire: development and validation of a multidimensional quality of life measure. J. Urol. 169, 1060–1064 (2003).
Giannarini, G. et al. Predictors of morbidity in patients with indwelling ureteric stents: results of a prospective study using the validated Ureteric Stent Symptoms Questionnaire. BJU Int. 107, 648–654 (2011).
Al-Kandari, A. M. et al. Effects of proximal and distal ends of double-J ureteral stent position on postprocedural symptoms and quality of life: a randomized clinical trial. J. Endourol. 21, 698–702 (2007).
Chew, B. H. et al. Pilot study of ureteral movement in stented patients: first step in understanding dynamic ureteral anatomy to improve stent comfort. J. Endourol. 21, 1069–1075 (2007).
Ramsay, J. W. et al. The effects of double J stenting on unobstructed ureters. An experimental and clinical study. Br. J. Urol. 57, 630–634 (1985).
Venkatesh, R. et al. Impact of a double-pigtail stent on ureteral peristalsis in the porcine model: initial studies using a novel implantable magnetic sensor. J. Endourol. 19, 170–176 (2005).
Kinn, A. C. & Lykkeskov-Andersen, H. Impact on ureteral peristalsis in a stented ureter. An experimental study in the pig. Urol. Res. 30, 213–218 (2002).
Dunn, C. J., Matheson, A. & Faulds, D. M. Tamsulosin: a review of its pharmacology and therapeutic efficacy in the management of lower urinary tract symptoms. Drugs Aging 19, 135–161 (2002).
Davenport, K., Timoney, A. G. & Keeley, F. X. A comparative in vitro study to determine the beneficial effect of calcium-channel and α1-adrenoceptor antagonism on human ureteric activity. BJU Int. 98, 651–655 (2006).
Rajpathy, J. et al. An in vitro study on human ureteric smooth muscle with the α1-adrenoceptor subtype blocker, tamsulosin. BJU Int. 102, 1743–1745 (2008).
Damiano, R. et al. Effect of tamsulosin in preventing ureteral stent-related morbidity: a prospective study. J. Endourol. 22, 651–656 (2008).
Wang, C. J., Huang, S. W. & Chang, C. H. Effects of specific α-1A/1D blocker on lower urinary tract symptoms due to double-J stent: a prospectively randomized study. Urol. Res. 37, 147–152 (2009).
Beddingfield, R. et al. Alfuzosin to relieve ureteral stent discomfort: a prospective, randomized, placebo controlled study. J. Urol. 181, 170–176 (2009).
Deliveliotis, C. et al. Is there a role for α1-blockers in treating double-J stent-related symptoms? Urology 67, 35–39 (2006).
Damiano, R. et al. Does the size of ureteral stent impact urinary symptoms and quality of life? A prospective randomized study. Eur. Urol. 48, 673–678 (2005).
Erturk, E., Sessions, A. & Joseph, J. V. Impact of ureteral stent diameter on symptoms and tolerability. J. Endourol. 17, 59–62 (2003).
Pryor, J., Carey, P. & Lippert, M. Migration of silicone ureteral catheters. J. Endourol. 2, 283–286 (1988).
Jeon, S. S., Choi, Y. S. & Hong, J. H. Determination of ideal stent length for endourologic surgery. J. Endourol. 21, 906–910 (2007).
el-Faqih, S. R. et al. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times. J. Urol. 146, 1487–1491 (1991).
Nagele, U., Praetorius, M., Schilling, D., Stenzl, A. & Anastasiadis, A. G. Comparison of flexible grasping forceps and stone basket for removal of retracted ureteral stents. J. Endourol. 20, 418–422 (2006).
Livadas, K. E. et al. Ureteroscopic removal of mildly migrated stents using local anesthesia only. J. Urol. 178, 1998–2001 (2007).
LeRoy, A. J., Williams, H. J. Jr, Segura, J. W., Patterson, D. E. & Benson, R. C. Jr. Indwelling ureteral stents: percutaneous management of complications. Radiology 158, 219–222 (1986).
Kehinde, E. O. et al. Bacteriology of urinary tract infection associated with indwelling J ureteral stents. J. Endourol. 18, 891–896 (2004).
Reid, G., Denstedt, J. D., Kang, Y. S., Lam, D. & Nause, C. Microbial adhesion and biofilm formation on ureteral stents in vitro and in vivo. J. Urol. 148, 1592–1594 (1992).
Schierholz, J. M., Beuth, J. & Pulverer, G. Silver coating of medical devices for catheter-associated infections? Am. J. Med. 107, 101–102 (1999).
Tieszer, C., Reid, G. & Denstedt, J. Conditioning film deposition on ureteral stents after implantation. J. Urol. 160, 876–881 (1998).
Elwood, C. N. et al. Understanding urinary conditioning film components on ureteral stents: profiling protein components and evaluating their role in bacterial colonization. Biofouling 29, 1115–1122 (2013).
Shaw, G. L., Choong, S. K. & Fry, C. Encrustation of biomaterials in the urinary tract. Urol. Res. 33, 17–22 (2005).
Klis, R., Korczak-Kozakiewicz, E., Denys, A., Sosnowski, M. & Rozanski, W. Relationship between urinary tract infection and self-retaining double-J catheter colonization. J. Endourol. 23, 1015–1019 (2009).
Kehinde, E. O. et al. Factors predisposing to urinary tract infection after J ureteral stent insertion. J. Urol. 167, 1334–1337 (2002).
Farsi, H. M., Mosli, H. A., Al-Zemaity, M. F., Bahnassy, A. A. & Alvarez, M. Bacteriuria and colonization of double-pigtail ureteral stents: long-term experience with 237 patients. J. Endourol. 9, 469–472 (1995).
Singh, I. et al. Severely encrusted polyurethane ureteral stents: management and analysis of potential risk factors. Urology 58, 526–531 (2001).
Tunney, M. M., Keane, P. F., Jones, D. S. & Gorman, S. P. Comparative assessment of ureteral stent biomaterial encrustation. Biomaterials 17, 1541–1546 (1996).
Gorman, S. P. & Tunney, M. M. Assessment of encrustation behaviour on urinary tract biomaterials. J. Biomater. Appl. 12, 136–166 (1997).
Tunney, M. M., Keane, P. F. & Gorman, S. P. Assessment of urinary tract biomaterial encrustation using a modified Robbins device continuous flow model. J. Biomed. Mater. Res. 38, 87–93 (1997).
Rouprêt, M. et al. Can ureteral stent encrustation analysis predict urinary stone composition? Urology 66, 246–251 (2005).
Canales, B. K. et al. Presence of five conditioning film proteins are highly associated with early stent encrustation. J. Endourol. 23, 1437–1442 (2009).
Olweny, E. O. et al. Evaluation of the use of a biodegradable ureteral stent after retrograde endopyelotomy in a porcine model. J. Urol. 167, 2198–2202 (2002).
Lam, J. S. & Gupta, M. Tips and tricks for the management of retained ureteral stents. J. Endourol. 16, 733–741 (2002).
Acosta-Miranda, A. M., Milner, J. & Turk, T. M. The FECal Double-J: a simplified approach in the management of encrusted and retained ureteral stents. J. Endourol. 23, 409–415 (2009).
Borboroglu, P. G. & Kane, C. J. Current management of severely encrusted ureteral stents with a large associated stone burden. J. Urol. 164, 648–650 (2000).
Ather, M. H., Talati, J. & Biyabani, R. Physician responsibility for removal of implants: the case for a computerized program for tracking overdue double-J stents. Tech. Urol. 6, 189–192 (2000).
Borin, J. F., Melamud, O. & Clayman, R. V. Initial experience with full-length metal stent to relieve malignant ureteral obstruction. J. Endourol. 20, 300–304 (2006).
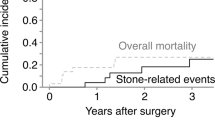
Kadlec, A. O., Ellimoottil, C. S., Greco, K. A. & Turk, T. M. Five-year experience with metallic stents for chronic ureteral obstruction. J. Urol. 190, 937–941 (2013).
Agrawal, S., Brown, C. T., Bellamy, E. A. & Kulkarni, R. The thermo-expandable metallic ureteric stent: an 11-year follow-up. BJU Int. 103, 372–376 (2009).
Liatsikos, E. N. et al. Ureteral metal stents: 10-year experience with malignant ureteral obstruction treatment. J. Urol. 182, 2613–2617 (2009).
Barbalias, G. A. et al. Metal stents: a new treatment of malignant ureteral obstruction. J. Urol. 158, 54–58 (1997).
Wakui, M., Takeuchi, S., Isioka, J., Iwabuchi, K. & Morimoto, S. Metallic stents for malignant and benign ureteric obstruction. BJU Int. 85, 227–232 (2000).
Hendlin, K., Korman, E. & Monga, M. New metallic ureteral stents: improved tensile strength and resistance to extrinsic compression. J. Endourol. 26, 271–274 (2012).
Sountoulides, P., Kaplan, A., Kaufmann, O. G. & Sofikitis, N. Current status of metal stents for managing malignant ureteric obstruction. BJU Int. 105, 1066–1072 (2010).
Kukreja, N., Onuma, Y., Daemen, J. & Serruys, P. W. The future of drug-eluting stents. Pharmacol. Res. 57, 171–180 (2008).
Kallidonis, P. S., Georgiopoulos, I. S., Kyriazis, I. D., Al-Aown, A. M. & Liatsikos, E. N. Drug-eluting metallic stents in urology. Indian J. Urol. 30, 8–12 (2014).
Krambeck, A. E. et al. A novel drug eluting ureteral stent: a prospective, randomized, multicenter clinical trial to evaluate the safety and effectiveness of a ketorolac loaded ureteral stent. J. Urol. 183, 1037–1042 (2010).
Mendez-Probst, C. E. et al. The use of triclosan eluting stents effectively reduces ureteral stent symptoms: a prospective randomized trial. BJU Int. 110, 749–754 (2012).
Kotsar, A. et al. Preclinical evaluation of new indomethacin-eluting biodegradable urethral stent. J. Endourol. 26, 387–392 (2012).
Liatsikos, E. N. et al. Application of paclitaxel-eluting metal mesh stents within the pig ureter: an experimental study. Eur. Urol. 51, 217–223 (2007).
Kallidonis, P. et al. Evaluation of zotarolimus-eluting metal stent in animal ureters. J. Endourol. 25, 1661–1667 (2011).
Al-Aown, A. et al. Ureteral stents: new ideas, new designs. Ther. Adv. Urol. 2, 85–92 (2010).
Venkatesan, N., Shroff, S., Jayachandran, K. & Doble, M. Polymers as ureteral stents. J. Endourol. 24, 191–198 (2010).
Chew, B. H. et al. Next generation biodegradable ureteral stent in a yucatan pig model. J. Urol. 183, 765–771 (2010).
Lingeman, J. E., Schulsinger, D. A. & Kuo, R. L. Phase I trial of a temporary ureteral drainage stent. J. Endourol. 17, 169–171 (2003).
Schlick, R. W. & Planz, K. Potentially useful materials for biodegradable ureteric stents. Br. J. Urol. 80, 908–910 (1997).
Schlick, R. W. & Planz, K. In vitro results with special plastics for biodegradable endoureteral stents. J. Endourol. 12, 451–455 (1998).
Lumiaho, J. et al. New bioabsorbable polylactide ureteral stent in the treatment of ureteral lesions: an experimental study. J. Endourol. 13, 107–112 (1999).
Lumiaho, J. et al. Drainage and antireflux characteristics of a biodegradable self-reinforced, self-expanding X-ray-positive poly-L,D-lactide spiral partial ureteral stent: an experimental study. J. Endourol. 21, 1559–1564 (2007).
Lumiaho, J. et al. The morphological, in situ effects of a self-reinforced bioabsorbable polylactide (SR-PLA 96) ureteric stent; an experimental study. J. Urol. 164, 1360–1363 (2000).
Li, G. et al. Introduction to biodegradable polylactic acid ureteral stent application for treatment of ureteral war injury. BJU Int. 108, 901–906 (2011).
Talja, M., Multanen, M., Välimaa, T. & Törmälä, P. Bioabsorbable SR-PLGA horn stent after antegrade endopyelotomy: a case report. J. Endourol. 16, 299–302 (2002).
Lumiaho, J., Heino, A., Aaltomaa, S., Välimaa, T. & Talja, M. A short biodegradable helical spiral ureteric stent provides better antireflux and drainage properties than a double-J stent. Scand. J. Urol. Nephrol. 45, 129–133 (2011).
Lingeman, J. E. et al. Use of a temporary ureteral drainage stent after uncomplicated ureteroscopy: results from a phase II clinical trial. J. Urol. 169, 1682–1688 (2003).
Hadaschik, B. A. et al. Investigation of a novel degradable ureteral stent in a porcine model. J. Urol. 180, 1161–1166 (2008).
Liatsikos, E. et al. Ureteral obstruction: is the full metallic double-pigtail stent the way to go? Eur. Urol. 57, 480–486 (2010).
Tsuji, T. et al. Biodegradable stents as a platform to drug loading. Int. J. Cardiovasc. Intervent. 5, 13–16 (2003).
Kotsar, A. et al. Biodegradable braided poly(lactic-co-glycolic acid) urethral stent combined with dutasteride in the treatment of acute urinary retention due to benign prostatic enlargement: a pilot study. BJU Int. 103, 626–629 (2009).
Amiel, G. E., Yoo, J. J., Kim, B. S. & Atala, A. Tissue engineered stents created from chondrocytes. J. Urol. 165, 2091–2095 (2001).
Nakayama, Y., Zhou, Y. M. & Ishibashi-Ueda, H. Development of in vivo tissue-engineered autologous tissue-covered stents (biocovered stents). J. Artif. Organs 10, 171–176 (2007).
Erbel, R. et al. Temporary scaffolding of coronary arteries with bioabsorbable magnesium stents: a prospective, non-randomised multicentre trial. Lancet 369, 1869–1875 (2007).
Author information
Authors and Affiliations
Contributions
All authors researched the data for the article and provided substantial contributions to discussions of its content. D.L., S.B. and N.H. wrote the article. D.L. and B.H.C. undertook review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
D.L. and B.H.C. declare consulting associations with Bard Medical, Boston Scientific, Cook Medical, Olympus and PercSys. S.B. and N.H. declare no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Lange, D., Bidnur, S., Hoag, N. et al. Ureteral stent-associated complications—where we are and where we are going. Nat Rev Urol 12, 17–25 (2015). https://doi.org/10.1038/nrurol.2014.340
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2014.340
This article is cited by
-
Mechanical characteristics of the ureter and clinical implications
Nature Reviews Urology (2024)
-
Effect of theophylline on stent-related symptoms in patients undergoing Double-J ureteral stent insertion: a randomized controlled trial
International Urology and Nephrology (2024)
-
Drug resistance and influencing factors of biofilm bacteria in upper urinary calculi patients with double J stent indwelling
BMC Urology (2023)
-
Efficacy and safety of combination of mirabegron and solifenacin in patients with double-J stent related overactive bladder: a prospective study
Scientific Reports (2022)
-
Influences of Stent Design on In-Stent Restenosis and Major Cardiac Outcomes: A Scoping Review and Meta-Analysis
Cardiovascular Engineering and Technology (2022)