Abstract
While over half of women with migraine report improvement during pregnancy, having a history of migraine may increase the chance of negative health outcomes. The state of pregnancy increases the risk of several dangerous secondary headache disorders, especially those associated with hypertensive disorders of pregnancy, and providers need to know the red flags to diagnose and treat emergently. Non-pharmacological migraine treatments can be instituted in advance of pregnancy as many are considered the safest options during pregnancy, but understanding the safety of medications and dietary supplements ensures appropriate care for the refractory migraine patient. New controversy exists over the safety of several historically routine and safe migraine treatment options in pregnancy, such as magnesium, acetaminophen, ondansetron, and butalbital. While it is not clear if breastfeeding decreases the postpartum recurrence of migraine, understanding safe treatment options during lactation can allow women to continue breastfeeding while achieving migraine relief.
Similar content being viewed by others
References
Kvisvik EV, Stovner LJ, Helde G, Bovim G, Linde M. Headache and migraine during pregnancy and puerperium: the MIGRA-study. J Headache Pain. 2011;12(4):443–51.
Sances G, Granella F, Nappi RE, Fignon A, Ghiotto N, Polatti F, et al. Course of migraine during pregnancy and postpartum: a prospective study. Cephalalgia. 2003;23(3):197–205.
Marcus DA. Headache in pregnancy. Curr Pain Headache Rep. 2003;7(4):288–96.
Marcus DA. Managing headache during pregnancy and lactation. Expert Rev Neurother. 2008;8(3):385–95.
Silberstein S. Sex hormones & headache. Philadelphia, PA: Current Medicine Group LLC, a division of Springer Science + Business Media LLC; 2007.
Granella F, Sances G, Pucci E, Nappi RE, Ghiotto N, Napp G. Migraine with aura and reproductive life events: a case control study. Cephalalgia. 2000;20(8):701–7.
Cupini LM, Matteis M, Troisi E, Calabresi P, Bernardi G, Silvestrini M. Sex-hormone-related events in migrainous females. A clinical comparative study between migraine with aura and migraine without aura. Cephalalgia. 1995;15(2):140–4.
Turner DP, Smitherman TA, Eisenach JC, Penzien DB, Houle TT. Predictors of headache before, during, and after pregnancy: a cohort study. Headache. 2012;52(3):348–62. This large longitudinal cohort study of pregnant women showed that those with a history of headache prior to pregnancy were at greater risk of experiencing headache during pregnancy.
Frederick IO, Qiu C, Enquobahrie DA, Aurora SK, Peterlin BL, Gelaye B, et al. Lifetime prevalence and correlates of migraine among women in a pacific northwest pregnancy cohort study. Headache. 2014;54(4):675–85.
Chen HM, Chen SF, Chen YH, Lin HC. Increased risk of adverse pregnancy outcomes for women with migraines: a nationwide population-based study. Cephalalgia. 2010;30(4):433–8.
Marozio L, Facchinetti F, Allais G, Nappi RE, Enrietti M, Neri I, et al. Headache and adverse pregnancy outcomes: a prospective study. Eur J Obstet Gynecol Reprod Biol. 2012;161(2):140–3.
Facchinetti F, Allais G, Nappi RE, D’Amico R, Marozio L, Bertozzi L, et al. Migraine is a risk factor for hypertensive disorders in pregnancy: a prospective cohort study. Cephalalgia. 2009;29(3):286–92.
Czerwinski S, Gollero J, Qiu C, Sorensen TK, Williams MA. Migraine-asthma comorbidity and risk of hypertensive disorders of pregnancy. J pregnancy. 2012;2012:858097.
Adeney KL, Williams MA, Miller RS, Frederick IO, Sorensen TK, Luthy DA. Risk of preeclampsia in relation to maternal history of migraine headaches. J Matern Fetal Neonatal Med. 2005;18(3):167–72.
Gelaye B, Larrabure-Torrealva GT, Qiu C, Luque-Fernandez MA, Peterlin BL, Sanchez SE, et al. Fasting lipid and lipoproteins concentrations in pregnant women with a history of migraine. Headache. 2015;55(5):646–57.
Wabnitz A, Bushnell C. Migraine, cardiovascular disease, and stroke during pregnancy: systematic review of the literature. Cephalalgia. 2015;35(2):132–9. This systematic review shows that women with a history of migraine have an increased risk of gestational hypertension, preeclampsia, ischemic stroke, acute myocardial infarction, heart disease, and thromboembolic events during pregnancy.
Qiu C, Frederick IO, Sorensen T, Aurora SK, Gelaye B, Enquobahrie DA, et al. Sleep disturbances among pregnant women with history of migraines: a cross-sectional study. Cephalalgia. 2015;35:1092.
Orta OR, Gelaye B, Qiu C, Stoner L, Williams MA. Depression, anxiety and stress among pregnant migraineurs in a pacific-northwest cohort. J Affect Disord. 2014;172c:390–6.
David PS, Kling JM, Starling AJ. Migraine in pregnancy and lactation. Curr Neurol Neurosci Rep. 2014;14(4):439.
Digre KB. Headaches during pregnancy. Clin Obstet Gynecol. 2013;56(2):317–29.
Brandes JL. Migraine in women. Continuum (Minneapolis, Minn). 2012;18(4):835–52.
Martin SR, Foley MR. Approach to the pregnant patient with headache. Clin Obstet Gynecol. 2005;48(1):2–11.
Robbins MS, Farmakidis C, Dayal AK, Lipton RB. Acute headache diagnosis in pregnant women: a hospital-based study. Neurology. 2015;85(12):1024–30. This retrospective review demonstrated that 35% of pregnant women presenting with an acute headache have a secondary headache disorder, suggesting the importance of neuroimaging and close monitoring in this population.
ACOG Committee on Obstetric Practice. ACOG Committee Opinion. Number 299, September 2004 (replaces No. 158, September 1995). Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004;104(3):647–51.
Schoen JC, Campbell RL, Sadosty AT. Headache in pregnancy: an approach to emergency department evaluation and management. West J Emerg Med. 2015;16(2):291–301.
Lee SY, Rhee CM, Leung AM, Braverman LE, Brent GA, Pearce EN. A review: Radiographic iodinated contrast media-induced thyroid dysfunction. J Clin Endocrinol Metab. 2015;100(2):376–83.
MacGregor EA. Migraine in pregnancy and lactation. Neurol Sci. 2014;35 Suppl 1:61–4.
Kesler A, Kupferminc M. Idiopathic intracranial hypertension and pregnancy. Clin Obstet Gynecol. 2013;56(2):389–96.
Digre KB, Varner MW, Corbett JJ. Pseudotumor cerebri and pregnancy. Neurology. 1984;34(6):721–9.
Bateman BT, Olbrecht VA, Berman MF, Minehart RD, Schwamm LH, Leffert LR. Peripartum subarachnoid hemorrhage: nationwide data and institutional experience. Anesthesiology. 2012;116(2):324–33.
Kasper EM, Hess PE, Silasi M, Lim KH, Gray J, Reddy H, et al. A pregnant female with a large intracranial mass: reviewing the evidence to obtain management guidelines for intracranial meningiomas during pregnancy. Surg Neurol Int. 2010;1:95.
Hayes AR, O’Sullivan AJ, Davies MA. A case of pituitary apoplexy in pregnancy. Endocrinol, Diabetes Metab Case Rep. 2014;2014:140043.
Piantanida E, Gallo D, Lombardi V, Tanda ML, Lai A, Ghezzi F, et al. Pituitary apoplexy during pregnancy: a rare, but dangerous headache. J Endocrinol Investig. 2014;37(9):789–97.
Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurology. 2012;11(10):906–17.
Klein AM, Loder E. Postpartum headache. Int J Obstet Anesth. 2010;19(4):422–30.
Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011;118(5):1102–7.
Hoshiyama E, Tatsumoto M, Iwanami H, Saisu A, Watanabe H, Inaba N, et al. Postpartum migraines: a long-term prospective study. Intern Med. 2012;51(22):3119–23.
Serva WA, Serva VM, Caminha Mde F, Figueiroa JN, Serva GB, Valenca MM. Exclusive breastfeeding protects against postpartum migraine recurrence attacks? Arq Neuropsiquiatr. 2012;70(6):428–34.
Airola G, Allais G, Castagnoli Gabellari I, Rolando S, Mana O, Benedetto C. Non-pharmacological management of migraine during pregnancy. Neurol Sci. 2010;31 Suppl 1:S63–5.
Mauskop A. Nonmedication, alternative, and complementary treatments for migraine. Continuum (Minneapolis, Minn). 2012;18(4):796–806.
Penzien DB, Irby MB, Smitherman TA, Rains JC, Houle TT. Well-established and empirically supported behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19(7):34. This paper provides an overview of the well-established and empirically supported behavioral interventions for the treatment of migraine, all very important treatment options during pregnancy.
Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128(1-2):111–27.
Nestoriuc Y, Martin A, Rief W, Andrasik F. Biofeedback treatment for headache disorders: a comprehensive efficacy review. Appl Psychophysiol Biofeedback. 2008;33(3):125–40.
Scharff L, Marcus DA, Turk DC. Maintenance of effects in the nonmedical treatment of headaches during pregnancy. Headache. 1996;36(5):285–90.
Int J Gynaecol Obstet. ACOG committee opinion. Exercise during pregnancy and the postpartum period. Number 267, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;77(1):79–81.
John PJ, Sharma N, Sharma CM, Kankane A. Effectiveness of yoga therapy in the treatment of migraine without aura: a randomized controlled trial. Headache. 2007;47(5):654–61.
Posadzki P, Ernst E, Terry R, Lee MS. Is yoga effective for pain? A systematic review of randomized clinical trials. Complement Ther Med. 2011;19(5):281–7.
Wells RE, Burch R, Paulsen RH, Wayne PM, Houle TT, Loder E. Meditation for migraines: a pilot randomized controlled trial. Headache. 2014;54(9):1484–95.
Jiang Q, Wu Z, Zhou L, Dunlop J, Chen P. Effects of yoga intervention during pregnancy: a review for current status. Am J Perinatol. 2015;32(6):503–14.
Narendran S, Nagarathna R, Narendran V, Gunasheela S, Nagendra HR. Efficacy of yoga on pregnancy outcome. J Altern Complement Med. 2005;11(2):237–44.
Gong H, Ni C, Shen X, Wu T, Jiang C. Yoga for prenatal depression: a systematic review and meta-analysis. BMC Psychiatry. 2015;15:14.
Beddoe AE, Lee KA, Weiss SJ, Kennedy HP, Yang CP. Effects of mindful yoga on sleep in pregnant women: a pilot study. Biol Res Nurs. 2010;11(4):363–70.
Davis K, Goodman SH, Leiferman J, Taylor M, Dimidjian S. A randomized controlled trial of yoga for pregnant women with symptoms of depression and anxiety. Complement Ther Clin Pract. 2015;21(3):166–72.
Peroutka SJ. What turns on a migraine? A systematic review of migraine precipitating factors. Curr Pain Headache Rep. 2014;18(10):454.
Satyapriya M, Nagendra HR, Nagarathna R, Padmalatha V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int J Gynaecol Obstet. 2009;104(3):218–22.
Bruehl S, Chung OY, Jirjis JN, Biridepalli S. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin J Pain. 2005;21(2):147–53.
Whitten CE, Donovan M, Cristobal K. Treating chronic pain: new knowledge, more choices. Perm J. 2005;9(4):9–18.
Govindappagari S, Grossman TB, Dayal AK, Grosberg BM, Vollbracht S, Robbins MS. Peripheral nerve blocks in the treatment of migraine in pregnancy. Obstet Gynecol. 2014;124(6):1169–74.
Silberstein SD. Migraine and pregnancy. Neurol Clin. 1997;15(1):209–31.
Content and format of labeling for human prescription drug and biological products; requirements for pregnancy and lactation labeling. Federal Register, the Daily Journal of the United States Government: FDA; [11-12-2015]. Available from: http://federalregister.gov/a/2014-28241.
Holland S, Silberstein SD, Freitag F, Dodick DW, Argoff C, Ashman E. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1346–53.
Hale TW, Rowe HE. Medications & mothers’ milk. 16th ed. Plano: Hale Publishing; 2014.
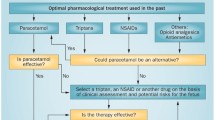
Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache. 2015;55(1):3–20.
Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1337–45.
Li DK, Liu L, Odouli R. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and risk of miscarriage: population based cohort study. BMJ. 2003;327(7411):368.
Loder E, Weizenbaum E, Frishberg B, Silberstein S. Choosing wisely in headache medicine: the American Headache Society’s list of five things physicians and patients should question. Headache. 2013;53(10):1651–9. This report recommends against the use of opioids and barbiturates for the treatment of migraines.
Lee RV. In: Burrow GN, Ferris TF, editors. Medical complications during pregnancy. 4th ed. Philadelphia, PA: WB Saunders Company; 1994.
Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC. In: Cunningham FG, MacDonald PC, Leveno KF, editors. Williams obstetrics. 19th ed. Norwalk, CT: Appleton & Lange; 1993.
Mangurten HH, Benawra R. Neonatal codeine withdrawal in infants of nonaddicted mothers. Pediatrics. 1980;65(1):159–60.
Loder E. Safety of sumatriptan in pregnancy: a review of the data so far. CNS Drugs. 2003;17(1):1–7.
Ephross SA, Sinclair SM. Final results from the 16-year sumatriptan, naratriptan, and treximet pregnancy registry. Headache. 2014;54(7):1158–72.
Marchenko A, Etwel F, Olutunfese O, Nickel C, Koren G, Nulman I. Pregnancy outcome following prenatal exposure to triptan medications: a meta-analysis. Headache. 2015;55(4):490–501.
Nezvalova-Henriksen K, Spigset O, Nordeng H. Triptan safety during pregnancy: a Norwegian population registry study. Eur J Epidemiol. 2013;28(9):759–69.
Hunt S, Russell A, Smithson WH, Parsons L, Robertson I, Waddell R, et al. Topiramate in pregnancy: preliminary experience from the UK Epilepsy and Pregnancy Register. Neurology. 2008;71(4):272–6.
Castilla-Puentes R, Ford L, Manera L, Kwarta Jr RF, Ascher S, Li Q. Topiramate monotherapy use in women with and without epilepsy: pregnancy and neonatal outcomes. Epilepsy Res. 2014;108(4):717–24.
Buettner C, Nir RR, Bertisch SM, Bernstein C, Schain A, Mittleman MA, et al. Simvastatin and vitamin D for migraine prevention: a randomized controlled trial. Ann Neurol. 2015;78:970.
Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med. 1998;338(16):1128–37.
Evers S, Afra J, Frese A, Goadsby PJ, Linde M, May A, et al. EFNS guideline on the drug treatment of migraine—revised report of an EFNS task force. Eur J Neurol. 2009;16(9):968–81.
Huang L, Bocek M, Jordan JK, Sheehan AH. Memantine for the prevention of primary headache disorders. Ann Pharmacother. 2014;48(11):1507–11.
Holden SC, Gardiner P, Birdee G, Davis RB, Yeh GY. Complementary and alternative medicine use among women during pregnancy and childbearing years. Birth. 2015;42(3):261–9.
Saper RB, Phillips RS, Sehgal A, Khouri N, Davis RB, Paquin J, et al. Lead, mercury, and arsenic in US- and Indian-manufactured Ayurvedic medicines sold via the Internet. Jama. 2008;300(8):915–23.
Dunlop AL, Gardiner PM, Shellhaas CS, Menard MK, McDiarmid MA. The clinical content of preconception care: the use of medications and supplements among women of reproductive age. Am J Obstet Gynecol. 2008;199(6 Suppl 2):S367–72.
Pringsheim T, Davenport W, Mackie G, Worthington I, Aube M, Christie SN, et al. Canadian Headache Society guideline for migraine prophylaxis. Can J Neurol Sci. 2012;39(2 Suppl 2):S1–59.
Tepper SJ. Nutraceutical and other modalities for the treatment of headache. Continuum (Minneapolis, Minn). 2015;21(4 Headache):1018–31.
Schurks M, Diener HC, Goadsby P. Update on the prophylaxis of migraine. Curr Treat Options Neurol. 2008;10(1):20–9.
Ma AG, Schouten EG, Zhang FZ, Kok FJ, Yang F, Jiang DC, et al. Retinol and riboflavin supplementation decreases the prevalence of anemia in Chinese pregnant women taking iron and folic acid supplements. J Nutr. 2008;138(10):1946–50.
Elsen C, Rivas-Echeverria C, Sahland K, Sanchez R, Molma L, Pahl L, et al. Vitamins E, A and B as possible risk factors for preeclampsia—under consideration of the PROPER study (“Prevention of Preeclampsia by High-Dose Riboflavin Supplementation”). Geburtshilfe Frauenheilkd. 2012;72(9):846–52.
Elsen C, Rivas-Echeverria C, Sahland K, Bogucki P, Rivas-Echeverria F, Molina L, et al. Prevention of preeclampsia by high dose riboflavin supplementation. Proc World Med Conf. 2011.
Teran E, Hernandez I, Nieto B, Tavara R, Ocampo JE, Calle A. Coenzyme Q10 supplementation during pregnancy reduces the risk of pre-eclampsia. Int J Gynaecol Obstet. 2009;105(1):43–5.
Loder E, Burch R, Rizzoli P. The 2012 AHS/AAN guidelines for prevention of episodic migraine: a summary and comparison with other recent clinical practice guidelines. Headache. 2012;52(6):930–45.
McGuffin M, Hobbs C, Upton R, Goldberg A, editors. American Herbal Products Association’s botanical safety handbook. Boca Raton: CRC Press LLC; 1997.
Lea R, Colson N, Quinlan S, Macmillan J, Griffiths L. The effects of vitamin supplementation and MTHFR (C677T) genotype on homocysteine-lowering and migraine disability. Pharmacogenet Genomics. 2009;19(6):422–8.
Menon S, Lea RA, Roy B, Hanna M, Wee S, Haupt LM, et al. Genotypes of the MTHFR C677T and MTRR A66G genes act independently to reduce migraine disability in response to vitamin supplementation. Pharmacogenet Genomics. 2012;22(10):741–9.
Sadeghi O, Nasiri M, Maghsoudi Z, Pahlavani N, Rezaie M, Askari G. Effects of pyridoxine supplementation on severity, frequency and duration of migraine attacks in migraine patients with aura: a double-blind randomized clinical trial study in Iran. Iranian J Neurol. 2015;14(2):74–80.
Salam RA, Zuberi NF, Bhutta ZA. Pyridoxine (vitamin B6) supplementation during pregnancy or labour for maternal and neonatal outcomes. Cochrane Database Syst Rev. 2015;6:Cd000179.
Generally recognized as safe (GRAS) substances database [Internet]. [cited October 23, 2015].
Slaughter SR, Hearns-Stokes R, van der Vlugt T, Joffe HV. FDA approval of doxylamine-pyridoxine therapy for use in pregnancy. N Engl J Med. 2014;370(12):1081–3.
Geiger CJ, Fahrenbach DM, Healey FJ. Bendectin in the treatment of nausea and vomiting in pregnancy. Obstet Gynecol. 1959;14:688–90.
McGuinness BW, Binns DT. ‘Debendox’ in pregnancy sickness. J R Coll Gen Pract. 1971;21(109):500–3.
Wheatley D. Treatment of pregnancy sickness. Br J Obstet Gynaecol. 1977;84(6):444–7.
Einarson TR, Leeder JS, Koren G. A method for meta-analysis of epidemiological studies. Drug Intell Clin Pharm. 1988;22(10):813–24.
McKeigue PM, Lamm SH, Linn S, Kutcher JS. Bendectin and birth defects: I. A meta-analysis of the epidemiologic studies. Teratology. 1994;50(1):27–37.
Nulman I, Rovet J, Barrera M, Knittel-Keren D, Feldman BM, Koren G. Long-term neurodevelopment of children exposed to maternal nausea and vomiting of pregnancy and diclectin. J Pediatr. 2009;155(1):45–50. e1-2.
FDA. FDA recommends against prolonged use of magnesium sulfate to stop pre-term labor due to bone changes in exposed babies 2013 [July 31, 2015]. Available from: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM353335.pdf. • The FDA no longer recommends IV magnesium for the treatment of pre-term labor in pregnancy and has changed its risk categorization from A to D during pregnancy.
Holcomb Jr WL, Shackelford GD, Petrie RH. Magnesium tocolysis and neonatal bone abnormalities: a controlled study. Obstet Gynecol. 1991;78(4):611–4.
Yokoyama K, Takahashi N, Yada Y, Koike Y, Kawamata R, Uehara R, et al. Prolonged maternal magnesium administration and bone metabolism in neonates. Early Hum Dev. 2010;86(3):187–91.
Lamm CI, Norton KI, Murphy RJ, Wilkins IA, Rabinowitz JG. Congenital rickets associated with magnesium sulfate infusion for tocolysis. J Pediatr. 1988;113(6):1078–82.
FDA. FDA drug safety communication: abnormal heart rhythms may be associated with use of Zofran (ondansetron) 2011 [Nov. 11, 2015]. Available from: http://www.fda.gov/Drugs/DrugSafety/ucm271913.htm.
FDA. Potential signals of serious risks/new safety information identified by the FDA Adverse Event Reporting System (FAERS) between January-March 2013. 2014.
Einarson A, Maltepe C, Navioz Y, Kennedy D, Tan MP, Koren G. The safety of ondansetron for nausea and vomiting of pregnancy: a prospective comparative study. BJOG. 2004;111(9):940–3.
Anderka M, Mitchell AA, Louik C, Werler MM, Hernandez-Diaz S, Rasmussen SA. Medications used to treat nausea and vomiting of pregnancy and the risk of selected birth defects. Birth Defects Res A Clin Mol Teratol. 2012;94(1):22–30.
Abstracts of the 29th International Conference on Pharmacoepidemiology & Therapeutic Risk Management. August 25-28, 2013. Montreal, Canada. Pharmacoepidemiology and drug safety. 2013;22 Suppl 1:1-521.
Pasternak B, Svanstrom H, Hviid A. Ondansetron in pregnancy and risk of adverse fetal outcomes. N Engl J Med. 2013;368(9):814–23.
Koren G. Treating morning sickness in the United States—changes in prescribing are needed. Am J Obstet Gynecol. 2014;211(6):602–6.
[11/6/2015]. Update on Motherisk Program at The Hospital for Sick Children. Available from: http://motherisk.org/women/commonDetail.jsp?content_id=1108.
Lipton RB, Baggish JS, Stewart WF, Codispoti JR, Fu M. Efficacy and safety of acetaminophen in the treatment of migraine: results of a randomized, double-blind, placebo-controlled, population-based study. Arch Intern Med. 2000;160(22):3486–92.
Werler MM, Mitchell AA, Hernandez-Diaz S, Honein MA. Use of over-the-counter medications during pregnancy. Am J Obstet Gynecol. 2005;193(3 Pt 1):771–7.
Brandlistuen RE, Ystrom E, Nulman I, Koren G, Nordeng H. Prenatal paracetamol exposure and child neurodevelopment: a sibling-controlled cohort study. Int J Epidemiol. 2013;42(6):1702–13.
Liew Z, Ritz B, Rebordosa C, Lee PC, Olsen J. Acetaminophen use during pregnancy, behavioral problems, and hyperkinetic disorders. JAMA Pediatr. 2014;168(4):313–20.
Migliore E, Zugna D, Galassi C, Merletti F, Gagliardi L, Rasero L, et al. Prenatal paracetamol exposure and wheezing in childhood: causation or confounding? PLoS One. 2015;10(8):e0135775.
Streissguth AP, Treder RP, Barr HM, Shepard TH, Bleyer WA, Sampson PD, et al. Aspirin and acetaminophen use by pregnant women and subsequent child IQ and attention decrements. Teratology. 1987;35(2):211–9.
Gilmore B, Michael M. Treatment of acute migraine headache. Am Fam Physician. 2011;83(3):271–80.
Silberstein SD. Migraine: preventive treatment. Curr Med Res Opin. 2001;17 Suppl 1:s87–93.
Goldman AS. Birth defects and drugs in pregnancy. Am J Hum Genet. 1977;29(5):546–8.
Browne ML, Van Zutphen AR, Botto LD, Louik C, Richardson S, Druschel CM. Maternal butalbital use and selected defects in the national birth defects prevention study. Headache. 2014;54(1):54–66.
Marcus DA, Scharff L, Turk DC. Nonpharmacological management of headaches during pregnancy. Psychosom Med. 1995;57(6):527–35.
Luedtke K, Allers A, Schulte LH, May A. Efficacy of interventions used by physiotherapists for patients with headache and migraine—systematic review and meta-analysis. Cephalalgia. 2015.
Bryans R, Descarreaux M, Duranleau M, Marcoux H, Potter B, Ruegg R, et al. Evidence-based guidelines for the chiropractic treatment of adults with headache. J Manip Physiol Ther. 2011;34(5):274–89.
Alcantara J, Cossette M. Intractable migraine headaches during pregnancy under chiropractic care. Complement Ther Clin Pract. 2009;15(4):192–7.
Wells RE. Spinal manipulation for headaches: will better quality trials do the trick? Headache. 2011;51(7):1149–51.
Green C, Martin CW, Bassett K, Kazanjian A. A systematic review of craniosacral therapy: biological plausibility, assessment reliability and clinical effectiveness. Complement Ther Med. 1999;7(4):201–7.
Fernandez-de-Las-Penas C, Alonso-Blanco C, Cuadrado ML, Miangolarra JC, Barriga FJ, Pareja JA. Are manual therapies effective in reducing pain from tension-type headache?: a systematic review. Clin J Pain. 2006;22(3):278–85.
Jakel A, von Hauenschild P. A systematic review to evaluate the clinical benefits of craniosacral therapy. Complement Ther Med. 2012;20(6):456–65.
Mataran-Penarrocha GA, Castro-Sanchez AM, Garcia GC, Moreno-Lorenzo C, Carreno TP, Zafra MD. Influence of craniosacral therapy on anxiety, depression and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. 2011;2011:178769.
Phillips CJ, Meyer JJ. Chiropractic care, including craniosacral therapy, during pregnancy: a static-group comparison of obstetric interventions during labor and delivery. J Manip Physiol Ther. 1995;18(8):525–9.
Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;21(1):Cd001218.
Neri I, Allais G, Schiapparelli P, Blasi I, Benedetto C, Facchinetti F. Acupuncture versus pharmacological approach to reduce hyperemesis gravidarum discomfort. Minerva Ginecol. 2005;57(4):471–5.
Park J, Sohn Y, White AR, Lee H. The safety of acupuncture during pregnancy: a systematic review. Acupunct Med. 2014;32(3):257–66.
Ashkenazi A, Matro R, Shaw JW, Abbas MA, Silberstein SD. Greater occipital nerve block using local anaesthetics alone or with triamcinolone for transformed migraine: a randomised comparative study. J Neurol Neurosurg Psychiatry. 2008;79(4):415–7.
Blumenfeld A, Ashkenazi A, Napchan U, Bender SD, Klein BC, Berliner R, et al. Expert consensus recommendations for the performance of peripheral nerve blocks for headaches—a narrative review. Headache. 2013;53(3):437–46.
(WHO) WHO. Breastfeeding health topics [October 19, 2015]. Available from: http://www.who.int/topics/breastfeeding/en/.
Johnston M, Landers S, Noble L, Szucs K, Viehmann L. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–41.
Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2012;8:Cd003517.
Duffy LC, Byers TE, Riepenhoff-Talty M, La Scolea LJ, Zielezny M, Ogra PL. The effects of infant feeding on rotavirus-induced gastroenteritis: a prospective study. Am J Public Health. 1986;76(3):259–63.
Dewey KG, Heinig MJ, Nommsen-Rivers LA. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr. 1995;126(5 Pt 1):696–702.
Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128(1):103–10.
Sachs HC. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013;132(3):e796–809.
American Academy of Pediatrics Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics. 2001;108(3):776–89.
Drugs and lactation database [Internet]. Available from: http://toxnet.nlm.nih.gov/newtoxnet/lactmed.htm.
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349(12):1157–67.
Hutchinson S, Marmura MJ, Calhoun A, Lucas S, Silberstein S, Peterlin BL. Use of common migraine treatments in breast-feeding women: a summary of recommendations. Headache. 2013;53(4):614–27.
Wojnar-Horton RE, Hackett LP, Yapp P, Dusci LJ, Paech M, Ilett KF. Distribution and excretion of sumatriptan in human milk. Br J Clin Pharmacol. 1996;41(3):217–21.
Budzynska K, Gardner ZE, Low Dog T, Gardiner P. Complementary, holistic, and integrative medicine: advice for clinicians on herbs and breastfeeding. Pediatr Rev. 2013;34(8):343–52. quiz 52-3.
Giuliani M, Grossi GB, Pileri M, Lajolo C, Casparrini G. Could local anesthesia while breast-feeding be harmful to infants? J Pediatr Gastroenterol Nutr. 2001;32(2):142–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rebecca Erwin Wells, Dana P. Turner, Michelle Lee, Laura Bishop, and Lauren Strauss declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Headache