Abstract
Background
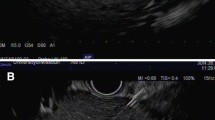
Diagnosis of metastatic disease is important in patients with cirrhosis and hepatocellular carcinoma (HCC) to prevent futile liver transplantation. Some of these patients have metastatic lymphadenopathy; however, it is difficult to perform percutaneous fine-needle aspiration due to presence of collateral and anatomic location. Endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) of lymph nodes offers several advantages like real-time vision, proximity to target, and avoidance of collaterals.
Aim
The aim of this study was to look for metastatic lymphadenopathy by EUS-guided FNA (EUS-FNA) in prospective liver transplant recipients with HCC.
Methods
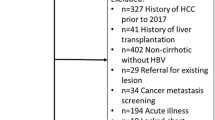
A prospective study was conducted from January 2013 to January 2016 at a tertiary care center. All prospective liver transplant recipients with HCC had PET-CT and bone scan to look for metastatic disease. EUS-FNA was done in patients with abdominal or mediastinal lymphadenopathy and no evidence of extrahepatic disease. Data is shown as median (25–75 interquartile range).
Results
EUS-guided FNA was done for 50 patients (42 abdominal and 8 mediastinal lymph nodes), age 57 (53–62) years, Child-Turcotte-Pugh 7 (6–9), and model for end-stage liver disease 10 (7–16). FNA material was adequate in 92% patients, metastasis in 15 (30%), granulomatous lymphadenopathy in 4 (8%), and reactive change in 27 patients (54%). The material was inadequate for diagnosis in 4 (8%) patients. Thus, EUS-guided FNA precluded transplantation in 30% of patients with lymphadenopathy, and 4 (8%) patients received anti-tubercular therapy before liver transplantation.
Conclusion
In patients with HCC and lymphadenopathy, EUS-guided FNA detected metastatic disease and precluded liver transplantation in approximately one third of patients.

Similar content being viewed by others
References
Kakodkar R, Soin AS. Liver transplantation for HCC: a review. Indian J Surg. 2012;74:100–17.
Bhangui P, Laurent A, Amathieu R, Azoulay D. Assessment of risk for non-hepatic surgery in cirrhotic patients. J Hepatol. 2012;57:874–84.
European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–43.
Dhir V, Mohandas KM. Epidemiology of digestive tract cancers in India. III Liver. Indian J Gastroenterol. 1998;17:100–3.
Yuen MF, Hou JL, Chutaputti A, Asia Pacific Working Party on Prevention of Hepatocellular Carcinoma. Hepatocellular carcinoma in the Asia pacific region. J Gastroenterol Hepatol. 2009;24:346–53.
Xiaohong S, Huikai L, Feng W, Ti Z, Yunlong C, Qiang L. Clinical significance of lymph node metastasis in patients undergoing partial hepatectomy for hepatocellular carcinoma. World J Surg. 2010;34:1028–33.
Kimura H, Matsubayashi H, Fukutomi A, et al. Lymph node metastasis diagnosed by EUS-FNA in four cases with hepatocellular carcinoma. Clin Res Hepatol Gastroenterol. 2011;35:237–40.
Lai R, Stephens V, Bardales R. Diagnosis and staging of hepatocellular carcinoma by EUS-FNA of a portal vein thrombus. Gastrointest Endosc. 2004;59:574–7.
Puli SR, Batapati Krishna Reddy J, Bechtold ML, et al. Endoscopic ultrasound: it’s accuracy in evaluating mediastinal lymphadenopathy? A meta-analysis and systematic review. World J Gastroenterol. 2008;14:3028–37.
Al-Haddad M, Wallace MB, Woodward TA, et al. The safety of fine-needle aspiration guided by endoscopic ultrasound: a prospective study. Endoscopy. 2008;40:204–8.
Acknowledgements
The authors want to express their heartfelt gratitude to the following people: Mr. Yogesh Saini, Ms. Payal Arora (research coordinators), and Mr. Mansih K Singh (biostatistician at Medanta).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
NSC, RP, SS, PB, NS, VS, MN, HS, MG, RS, and ASS declare that they have no conflict of interest.
Ethics statement
The authors declare that the study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning Human and Animal Rights, and the authors followed the policy concerning Informed Consent as shown on Springer.com.
Rights and permissions
About this article
Cite this article
Choudhary, N.S., Puri, R., Saigal, S. et al. Impact of endoscopic ultrasound-guided fine-needle aspiration in prospective liver transplant recipients with hepatocellular carcinoma and lymphadenopathy. Indian J Gastroenterol 35, 465–468 (2016). https://doi.org/10.1007/s12664-016-0718-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-016-0718-0